Your cart is currently empty!
Category: Pain

5 Hip Impingement Exercises to Relieve Your Hip Pain
Hip pain can hold you back from many activities: from your favorite sports, to games with the kids, or even hitting it hard at the gym. Finding the root of your hip pain is the first step to doing something about it.
If you suspect (or know) that your pain stems from hip impingement, introducing hip impingement exercises to your routine may also help you address and treat your pain.
What is hip impingement syndrome?
Also known as femoroacetabular impingement (FAI), hip impingement syndrome is when the contact point of the hip joint (the ball and socket) has abnormal wear and tear. It is technically a mechanical or structural disorder that directly impacts the hip joint.
Usually, this wear on the hip joint occurs on the labrum (or hip joint cartilage) and develops over time due to excess friction on the joint structure. The added friction could be caused by overuse, incorrect form when exercising, tight hip flexor muscles, or an abnormal hip shape. Any of these reasons has been known to cause hip impingement pain.
In a healthy, normally functioning hip, the top of the thigh bone (the femoral head) is rounded to fit perfectly into the hip socket (the acetabular socket). When this is a seamless fit, the femoral head can move without resistance.
There is a thin layer of smooth cartilage that protects these bones at their connection point and a labrum around the rim of the hip socket creating a protective ridge of cartilage for added security during femoral head movement.
Anytime something prevents this smooth, seamless movement between the hip’s femoral head and the acetabular socket, hip impingement may occur.
Hip impingement syndrome symptoms can affect anyone at any age – even young adults and children.
Bone shape, tight muscles, and hip impingement pain
When we think about hips and hip injuries, we often assume that everyone’s hip is precisely the same. But, just like we all have varying body shapes, our hip bone shapes and hip joints are different, too.
Being aware of your unique hip bone shape can be one of the most effective ways to set realistic expectations for your body, especially if you’re an athlete. For example, one person may have an extremely shallow hip socket. Shallow hip sockets will allow for more mobility and flexibility, but they may also create instability and a higher chance of labrum damage, hip labrum tears, and pain from hip impingement.
The human body has a fantastic way of working extra hard to correct injured areas. So as hip impingement sets in for most people, the iliopsoas muscles begin to tighten. These muscles are what you might think of as your hip flexor muscles, and they connect your spine and pelvic bone to the inside of your femur (thigh bone), facilitating movement and giving your body stability.
The iliopsoas muscle is actually made up of two large muscles that sit side-by-side: the iliacus and psoas. These two muscles help stabilize the pelvis and core with every movement you make – whether sitting, standing, bending over to tie your shoe, or stretching out your legs after a long day. They also help protect the hip joint and tendons in your body from taking on too much stress.
But when a damaged hip or hip joint is thrown into the mix, the iliopsoas muscles become fatigued. This may result in tightness in your hip flexors and/or hip pain. And, as your iliopsoas muscles begin to tighten and pull on the bones they connect to, that can cause a pelvic tilt, difficulty fully extending your legs, lower back pain, and a host of other issues. This is what we refer to as a “twisted core.” It’s the result of one or both of your iliopsoas muscles refusing to loosen their grip on your body.
As you can imagine, having tight hip flexors can also make hip impingement symptoms even worse. Having your hips out of alignment can cause problems on its own. Paired with already existing hip impingement syndrome, tight iliopsoas muscles are likely to create even more friction during movement.
In order to ease hip impingement pain, and find the correct hip impingement exercises for your case, it’s important to understand the type of impingement you are dealing with.
Types of hip impingement
The exact type of hip impingement you’re experiencing has a lot to do with the shape of your hip joint bones. There are two main types of hip impingement that doctors will often refer to.
- Cam impingement: This occurs when the ball-shaped end of the femur is not perfectly round. Since the femoral head has an abnormal shape, the way it rubs as it moves in the socket adds extra friction to the cartilage and labrum.
- Pincer impingement: This happens when the femoral head is covered too much by the acetabulum or socket. This excess coverage can cause the femur’s neck to touch and impinge along the rim of the hip socket. Over time, this causes cartilage and labral damage.
Just because you have one type of impingement in your hip doesn’t mean you can’t have the other. Plus, there are even more types of impingement than these two. These are simply the most commonly referred to by doctors.
In the absence of both cam and pincer impingement, hip impingement caused by hypermobility or a shallow hip socket is also possible.
To understand if you have hip impingement and could benefit from hip impingement exercises, let’s take a look at some of the symptoms of this syndrome.
Hip impingement symptoms
Hip impingement symptoms often fly under the radar for years. Some people won’t even feel pain until the hip damage worsens with time. The most common symptom is pain in the groin area. However, pain may not be existent at all in the early stages of hip impingement, or you may associate it with other issues.
Hip impingement pain will usually be more noticeable when walking, running, or performing an exercise that flexes the hip.
Other than hip pain, you may experience some decreased range of motion and tightness in the iliopsoas muscles.
When hip impingement symptoms first occur, you may only feel resistance, pain, or decreased range of motion when engaging in stretching, running, jumping, or other activities that put stress on the hip joint.
So, if you’re an athlete that often pushes the limits of your body, you may notice hip impingement pain much earlier than someone that works in an office setting and goes on leisurely walks each evening.
No matter the hip engagement, if the syndrome worsens with time and day-to-day hip use, even the most simple activities could become painful. Doing things like walking up stairs or standing up from sitting after driving to the market are likely to produce pain in the groin area.
Something that hip impingement patients need to realize is that if gone unchecked, hip impingement can lead to osteoarthritis.
If you are having pain at night as you are lying in bed, or even when walking slowly on flat ground, this could mean that a lack of cartilage is allowing contact of the bones as you move. As the cartilage breaks down, other symptoms could arise, and osteoarthritis is not out of the question.
Now that you are aware of the symptoms, it’s time to explore some hip impingement exercises to properly stabilize your hip joints and prevent hip pain.
Top 5 hip impingement exercises
Luckily, surgery is not the first or only option to treat hip impingement. While some patients may require surgery due to severe damage to the labrum or joint structure, we believe it should be a last resort.
Instead, we focus on helping you create and practice hip impingement exercises that strengthen the muscles around your hip joint and promote balance and alignment.
Here are the top five hip impingement exercises to try before resorting to surgery.
1. Stretching
When entering into physical therapy for hip impingement of any kind, it is essential to note that strength training and stretching are equally important. If you try to rely solely on stretching, it is possible to overstretch your hip muscles – especially the iliopsoas.
Since hip impingement can be caused by hyper flexibility, overstretching your hip flexor muscles could exacerbate the problem entirely. Still, if part of your hip’s misalignment is from overly tight muscles, then some hip stretching could be beneficial.
Knowing the cause and type of your hip impingement can help your physical therapist design hip impingement exercises that will not be harmful to your joint.
Some commonly used stretches that a physical therapist may have you do include:
- Hip flexor stretches like lunges
- Groin stretches like a gentle butterfly stretch
- Piriformis stretches to stretch the back hip
Be sure to listen to your body as you engage with these hip impingement exercises. Happy muscles shouldn’t hurt. Tightness and pain are both indicators that you could be stretching your muscles too far.
2. Core strengthening
Besides stretching the iliopsoas muscles, strength training will often be used to further stabilize the hip structure and keep it in proper alignment. Hip strengthening may seem normal in this situation, but what about core strengthening as part of your hip impingement exercises?
Your iliopsoas muscles are a part of your core and play a large role in the stability of not just your hips, but your whole body. So, by balancing out the muscle strength in and around your hips, you add more stability to the hip joint itself.
Core strengthening exercises ideal for hip impingement patients:
- Bridging
- Leg raises
- Pelvic tilt
- Pelvic clock
Just as with stretching exercises, if core strengthening exercises cause you pain at any time, STOP. Be sure to report these instances back to your physical therapist so they can restructure hip impingement exercises that better fit your needs.
3. Hip strengthening
Since your hip area is the source of your pain, it’s important to strengthen your hip region. Of course, finding hip-strengthening exercises that don’t hurt may take some trial and error. You may also need to work with your therapist to release your muscles and promote the correct hip joint alignment before engaging in any strengthening movements or exercises.
One way to do this is with a tool like the Hip Hook, the only muscle release tool designed to release both the psoas and the hard-to-reach iliacus muscle. The iliacus is half of your iliopsoas, and it is too often overlooked in addressing hip pain and impingement. Its location along the inner side of your pelvic muscle can make it very difficult to reach and release without a specific tool or a skilled therapist.
Once you’ve used the Hip Hook and felt a release, you can then move to some of these hip impingement exercises that may help strengthen the hips:
- Bridges (single and double leg)
- Clamshells
- Lateral band walking
- Isometric hip raise
- Hip hikes
Remember, releasing muscle tension needs to happen before you can strengthen. Otherwise, you will cause your already-tight muscle to contract even more or may not be able to achieve a full range of motion.
4. Balance exercises
Many balance exercises may feel a bit like strength training and will engage your leg muscles, hip muscles, glutes, and core. Working on balance is a way to target small muscle groups around the hip joint to improve the joint’s stability. As your balance improves, you will gain more control of your pelvic and lower extremities, and take some pressure off of the hip joint itself.
Keep in mind that when performing balance exercises, you will have to push yourself just a little. If it’s easy to balance, try to move to the next level of a movement, or shift the position of your eyes. Feeling wobbly is normal!
Balance exercises to try include:
- Using a Bosu ball
- Standing on a balance board
- Single leg squats
When attempting these hip impingement exercises, be sure to have something nearby (such as a wall or chair) to help you with stability as needed. Work to find a balance of challenging yourself just enough to pursue a better balance, without putting yourself in danger of injury.
And, if you are unsure of any movement, always ask your therapist. They will be there to supervise your form and provide alternatives if your current level of hip mobility doesn’t allow you to safely do an exercise.
5. Working on form and functional training
Something as simple as the way you step as you walk can impact your hips. Body awareness is important for managing and treating hip joint pain.
Functional training will teach your body how to move correctly as you go about day-to-day activities. This can also be targeted to your needs. For instance, if you’re an athlete, you may need functional training to strengthen your hip joint enough for sprinting or kicking. If that’s the case, a physical therapist would need to structure your hip impingement exercises around your form and overall awareness of movement.
And when doing any of the above hip impingement exercises, you should always prioritize form over trying to go deeper into a stretch or completing an exercise more quickly. In many ways, you are re-teaching your body and hips to move in a different way while doing familiar exercises. If you’ve been suffering from hip impingement for some time, your body may have acquired muscle memory around improper form. This may be as a result of certain muscles compensating for others in your hip region or because your hip joint structure wouldn’t allow for a full range of motion.
So, be gentle with yourself! Slow down and listen to your body.
Other hip impingement treatment options
Though these solutions may help, remember that hip impingement exercises aren’t everything. While physical therapy is the ideal option for treating hip impingement, some other options are available. Things like rest, pressure release of muscles, injections, and surgery could all be a part of the healing process.

7 Home Remedies for Sacroiliac Joint Pain
If you’ve ever felt lower back pain, hip pain, or other pelvic joint pain, then you may also have experienced — or still be experiencing — sacroiliac joint pain.
Your pelvis, hips, tailbone, and spine are a very complex and vital part of your ability to function during your day-to-day activities. One part of this system is your sacroiliac joint, which makes small yet important movements with every one of your steps. So, what happens when those joints cause you pain?
While surgery is sometimes necessary for sacroiliac joint pain, home remedies for sacroiliac joint pain also exist and can be quite useful when applied correctly. You should also consult a medical physician before implementing specific exercises or heath routines into your life.
There are a million home remedies out there on the internet, and not all of them are created equal. To help narrow down your search — and save you time and effort — I’ve put together a list of home remedies for sacroiliac joint pain that actually work.
Before we get started though, it would be helpful for you to understand more about the sacroiliac joint and how it affects your body.
What is the sacroiliac joint?
Your SI (sacroiliac) joint is where your sacrum connects to the ilium bones, and is located directly above the tailbone and is mostly immobile, allowing only four degrees of rotation. There are many soft tissues (muscles, ligaments, cartilage) that hold the SI joint in alignment and support movement. Because of the close proximity to your hips and tailbone, the SI joint is still necessary for completing everyday movements as it balances and absorbs shock from walking or jumping in the spine.
The SI joint is a self-locking joint, so it locks whenever you prepare to perform an activity like jumping or running. Since it functions so frequently during daily movements, your SI joint endures a lot of stress and tension.
For your body to perform all of the movements absorbed by the SI joint, you engage your iliopsoas muscles, commonly known as your hip flexors. You can think of the iliopsoas muscles as the puppet masters of your hip and pelvic joints and bones.
The iliacus and psoas muscles that make up the iliopsoas grab hold of your pelvis and thigh bones and help them engage in movements like sitting, standing, or kicking. These muscles work hand-in-hand with your SI joint to create comfortable movement, but they don’t always work as planned.
How to recognize sacroiliac joint pain
SI joint dysfunction has become increasingly common due to the immense stress the joint goes through day to day. However, because of its location, it can be challenging to identify where your pain is originating from, or if it is an SI joint dysfunction at all.
If you are struggling with SI joint dysfunction, pain is most often identified in the lower back region. There are plenty of other possible symptoms of sacroiliac joint pain, including:
- Difficulty balancing
- A slight burning sensation near your pelvis
- General pain in your hips, groin, or thighs
- Trouble sleeping due to discomfort in your back or hips
- Pain after sitting for long periods
Many people who experience SI joint pain will experience symptoms like those listed above in the morning after being immobile for the night, or during physical activity. Certain activities like walking up and down stairs or doing squats can also trigger intense pain, as they further engage your iliopsoas muscles and pelvic area
Common causes of sacroiliac joint pain
Since your iliopsoas muscles essentially utilize the SI joint, it is important to recognize that hip joint, pelvic joint, and SI joint pain are often associated with tight iliopsoas muscles. Since the iliopsoas muscles work in tandem with your pelvic joints, including the SI joint, if your muscles are tight, they directly impact these joints.
The primary function of the iliacus is to stabilize the hip joint and the sacroiliac joint (or SI joint), keeping those two joints aligned and strong regardless if the body is stationary (such as when sitting or standing) or if the body is moving (such as when walking or running). Other secondary functions of the iliacus include assisting in hip flexion (like marching) and hip external rotation (turning out your leg). Your body is the most comfortable when your spine, pelvis, and hips are aligned, working together with the iliopsoas muscles.
It helps to think of the iliopsoas muscles like a rubber band holding a stack of cards together. Without healthy and fully-functioning iliopsoas muscles, your hip, spine, and pelvis alignment can easily topple out of place, like a deck of cards — causing pain in your back, hips, and SI joint. This misalignment affects the way the bones move in relation to each other, and if they’re not well-aligned then they are running into each other and rubbing each other the wrong way.
Now that you are aware of what the SI joint is, and some common causes for pain in that region, let’s look at some home remedies for sacroiliac joint pain so we can help you find sacroiliac joint pain relief.

Home remedies for sacroiliac joint pain
While sacroiliac joint pain treatments will vary according to the pain’s severity, many home remedies for sacroiliac joint pain can help ease symptoms.
It can be tempting to treat sacroiliac joint pain entirely at home, but it can help get the guidance of a medical professional and physical therapist. Some people will need interventions such as surgeries, steroid injections, or physical therapy.
For those who can get by without more serious treatments and interventions, here is my recommended list of home remedies for sacroiliac joint pain:
Anti-inflammatory medications
One of the fastest home remedies for sacroiliac joint pain is anti-inflammatories. A lot of sacroiliac pain is due to inflammation of your muscles and joint area. When you’re first addressing your pain and other symptoms, it may be necessary to use non-habit forming anti-inflammatory medications, especially after activities that may irritate your joints.
Ice and heat therapy
If you are looking for home remedies for sacroiliac joint pain that don’t require medication, one of the best is ice and heat therapy. As mentioned above, inflammation can be a huge issue with sacroiliac pain. While anti-inflammatory drugs can be beneficial, ice and heat therapy will also relax and relieve pain. It is most helpful to alternate between ice therapy and heat therapy. Start with ice therapy on the irritated area, or where you’re feeling the most pain, to bring down some of the swelling. Then, apply heat to the SI joint area to improve blood flow and relax the joint area to relieve some pain.
Losing weight
Some home remedies for sacroiliac joint pain require more long-term commitment. Anytime you carry excess weight in your body, you add extra stress to your joints. This is the same for your SI joint area. Excess weight, specifically on your abdomen area, adds a significant amount of stress on your spine, hip joints, pelvic joint, and the SI joints because they are working harder to keep your body upright and in a correct posture.
Losing excess weight will help keep your joints aligned, and minimize the stress put on them during daily activities. If you are experiencing back or SI joint pain, it can be difficult to motivate yourself to exercise. The good news is that weight can be lost and maintained with a healthy diet and low-impact exercise.
SI joint pain exercises
Working exercise into your routine is important for various health reasons, but finding specific SI joint pain exercises to incorporate into your daily routine can help strengthen, balance, and stretch the SI joint area.
Not all exercises are suitable for the SI joint, though, so remember that if it causes you pain to perform a stretch or exercise, listen to your body and stop. As you alleviate more of the SI joint pain, more exercises may become easier and more comfortable.
There are a variety of yoga poses that help both stretch and strengthen the SI joint area. They are great home remedies for sacroiliac joint pain. A few of the best joint pain exercises include:
- Cobra pose
- Child’s pose
- Bird dog
- Bridge
- Single and double knee to chest
- Hip and knee rolls side to side
Wear an SI joint brace
One of the most prevalent home remedies for sacroiliac joint pain, especially when dealing with severe SI joint pain, is to wear a sacroiliac joint belt or brace. The use of an SI joint belt is most common in people that experience SI joint pain and also have hypermobile joints. Sacroiliac joint belts support and compress the joint area, and prevent the joints from moving too much.
Luckily, most SI joint belts and braces are quite low profile and can be worn under clothing. However, the SI joint braces should not be seen as a long-term solution, simply as a stepping stone to provide some relief throughout the sacroiliac joint pain treatment process.
Eliminate inflammatory foods from your diet
If you are looking for dietary home remedies for sacroiliac joint pain, avoiding and minimizing your consumption of inflammatory foods can be helpful.
Highly inflammatory foods to avoid include:
- Sugar (including high fructose corn syrup)
- Vegetable and seed oil
- Artificial trans fats
- Alcohol
- Refined carbohydrates
- Processed meats
- Dairy
Along with avoiding inflammatory foods, you can also consider introducing more anti-inflammatory foods to your diet, including:
- Berries
- Broccoli
- Green tea
- Grapes
- Peppers
- Mushrooms
- Turmeric
- Cherries
Eating a whole foods, plant-based diet cuts out highly processed, sugary, and fried inflammatory foods and introduces more fruits and vegetables to your diet.
Iliopsoas muscle release
At this point, you may not be surprised that one of the most efficient home remedies for sacroiliac joint pain actually targets your iliopsoas muscles. Since the iliopsoas muscle is so intimately connected to your sacroiliac joints’ well-being and function, tight iliopsoas muscles can cause additional SI joint pain. Watch a video to understand more about how tight hip flexors affect SI joint pain.
Although some stretching can help, stretching alone won’t fully address muscle tightness and in some cases can worsen it. The best way to release these muscles is with precise, prolonged (30-90 seconds) pressure. Reaching your hip flexor muscles with average massage tools like foam rollers is very difficult because of the location. You may get some relief when going to the physical therapist because they can reach the iliopsoas muscle with their hands.
For the best iliopsoas muscle release results, you’ll need to use a tool designed specifically for releasing your hip flexors. Designed by a physical therapist, the only muscle release tool with the ability to effectively reach and release your psoas and iliacus muscles is the Hip Hook.
Once all the hip flexor muscles are released, you should notice a marked difference in your SI joint pain.

Piriformis muscle release
The piriformis is a muscle in the back of your hip, and easily found by laying on your back with your knees bent and placing a massage ball in the middle of your buttcheek. Allowing your muscles to relax over the Hip Flexor Release Ball for 30-90 seconds. You can use this to release tension in the back of the hip. When the piriformis becomes tight, it pulls on the sacrum and ilium and can lead to compression or misalignment around the SI joint. As you continue to move your body with these supporting muscles not functioning optimally, the sacrum and ilium rub each other the wrong way and cause the soft tissues inside the joint to become irritated.
A tight piriformis muscle often goes hand-in-hand with tight hip flexors, like your iliacus and psoas muscles. This is because your body is searching for balance on each side of the hip. If the hip flexors on the front of the hip are tight and pulling the pelvis, the muscles on the back side of the hip (like the piriformis) will tighten up and play a game of tug-of-war. This combination of a tight iliacus and tight piriformis is very common among people who are experiencing SI joint pain.

Are trigger points the cause of your muscle pain?
What are trigger points?
Myofascial trigger points (or simply “trigger points”) are contracted areas inside a muscle or surrounding connective tissue (called fascia) that stay shortened no matter what you’re doing. Also known as muscle knots, these areas can be very sensitive to pressure and cause pain.
While you could previously contract and relax that muscle, some of the muscle fibers are now outside your conscious control. It’s like the “on” button at the control center gets flipped and the controller goes out to lunch.
Trigger points are important to understand because sometimes we can feel pain in one area that is actually coming from a different location. Referred pain from trigger points is often felt in multiple locations. Localized pain is felt in the immediate area surrounding the muscle knot, while referred pain is felt elsewhere in the body.
What are latent trigger points?
A latent trigger point can be described as a tight area within the muscle tissue that is “hidden” beneath the surface, meaning that you don’t know it exists until it gets accidentally, or purposefully, pressed on. Because of this, it’s possible that one of these trigger points has existed in your body and remained unaddressed for a long period of time.
For example, let’s say you’re sitting at your desk and a friend swoops by and squeezes your shoulders around your upper traps (a common area to find trigger points on people), pressing their thumbs into the muscle. You’ll probably feel some pain (and possibly relief, if they hold that spot for at least 30 seconds) directly where they were pressing, but possibly also up into the neck and head area. If they pressed hard enough, you might even experience a headache from the pressure. You may not have noticed those spots before, but you’ll definitely notice them now!

What are active trigger points?
A latent trigger point can become an active trigger point if it’s rubbed, contracted, overstretched, or during periods of stress or dehydration. Active trigger points cause localized and referred pain patterns without being pressed on. Using the same example from above, you’d experience pain in the traps, neck, and head while simply sitting at your desk. No outside stimulus needed; it hurts all on its own. Having someone press on the active trigger point likely would increase the pain, but it exists regardless.
What are common symptoms of trigger points?
If you squeeze your shoulder with your hand and feel a dense ball of muscle (what we often call a muscle knot), you have found a trigger point. You can either do this yourself, or have a trained professional (such as a physical therapist or massage therapist) help you out in feeling for these spots. If you hold on to that point for a few seconds and with enough pressure, you may even feel that trigger point start to refer somewhere else.
Common trigger point symptoms may include (but are not limited to):
- Dull aching or muscle tenderness
- Muscle stiffness and reduced range of motion
- Muscle weakness or fatigue
- Involuntary muscle contractions (or twitches)
- Inability to get a muscle to relax
- Affected area feels “warm” to the touch
- Burning or tingling sensations
Because of latent and active myofascial trigger points, another tell-tale sign and common symptom of having a trigger point is experiencing local and/or referred pain patterns when having pressure applied to that area of your body.
Trigger points may mimic other conditions
Due to possible referred pain patterns, trigger point symptoms may mimic the symptoms of other conditions, such as:
- Sciatica
- Sacroiliac (SI) joint pain
- Iliotibial (IT) band syndrome
- Neck pain and tension headaches
- Temporomandibular joint (TMJ) pain
- Abdominal or pelvic pain
- Sexual dysfunction (including pain with intercourse)
- Low back pain, hip pain, and knee pain
- And so much more…
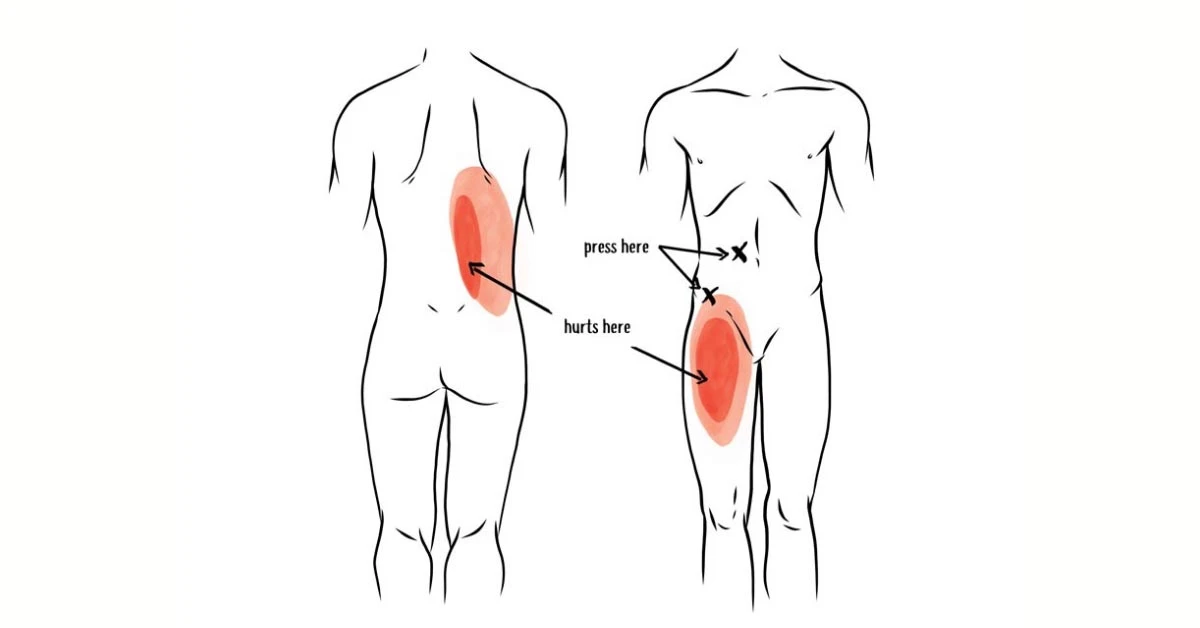
The below images show common patterns caused by trigger points, and why the root of the problem may not be where you’re feeling the pain. They’re also great examples of why trigger points can cause myofascial pain that may be mistaken for other conditions or diagnoses.

Iliacus trigger point & psoas trigger points
- iliacus trigger points refer pain to the anterior hip/thigh and groin, which may be mistaken for quadricep pain/tightness, hip arthritis or hip labrum issues
Gluteus minimus trigger points
- refer pain to the deep glute, outer hip, and down the leg, which may be mistaken for hip bursitis, IT band syndrome, or possibly even sciatica
Piriformis trigger points
- refer pain deep in the glute and down the back of the thigh, which may be mistaken for sciatica
Quadratus lumborum trigger points
- refer pain to the SI (sacroiliac) joint and glute (buttocks), which may be mistaken for SI joint pain or dysfunction
Because of this possibility, it is best to check with your healthcare practitioner for an evaluation of your pain to determine the root cause of your symptoms and set you up with an appropriate course of action to treat and improve the issue.
What causes trigger points?
Trigger points can develop as a result of muscles being used too much, contracted for a long time without relaxation, shortened too long, or in a stressful situation. Once a muscle is “on” for too long, the brain decides to keep that muscle contracted for good.
Poor posture can cause trigger points
Being in poor posture takes your body out of its natural alignment, making certain muscles work harder than they should to hold you in that position. For example, many people have rounded shoulders and a forward head posture. This makes the muscles in your upper back (in between the shoulder blades) and on the back side of your neck tighten up and hold tension to prevent the body from falling forward even more.
Inactivity can cause trigger points
As more and more of us slowly sink into our couches, it’s not a surprise when there is a myofascial component contributing to people’s pain. Spending lots of time consecutively in a stationary position (e.g. sitting, whether on an Ikea couch or a Herman Miller chair) does not challenge or strengthen the muscles in your body.
As this way of living continues consistently over time, it leaves your muscles in a weakened and unconditioned state to where they now begin to take on the shape and length of where they spend the majority of their time — in a seated, slouched, or distorted position.
Working on a computer can cause trigger points
Muscle knots in the tops of the shoulder area (upper trapezius) are common for people doing computer work. With your arms reaching out in front of the body all day long, the upper trapezius muscle is constantly “on” to prevent your shoulders from falling forward and to keep your head from rolling off your shoulders (and you thought your morning coffee was doing that!)
After a long day of work, this muscle will likely stay contracted when you‘re done typing. So even if you’re just walking the dog or making dinner, or relaxing on the couch, this muscle is stuck in the “on” position.
Sitting at a desk can cause trigger points
Sitting also results in the shortening and tightening of the body’s hip flexor muscles and ultimately the development of trigger points in the hip flexors that cause localized and referred pain in the body.
Muscular imbalances can cause trigger points
Your muscles hold your body in alignment, where there is a necessary relative relationship between the strength and length of the muscles on either side of your body — front vs. back and left vs. right — to remain in balance and function optimally.
For example, when the hip flexor muscles on the front side of your body tighten up and become shorter, this tilts your pelvis forward into an anterior position. The glute and hamstring muscles connect to the pelvis on the back side of your body, where they become longer than normal and weaken. It basically becomes a game of “tug-of-war” where those muscles now tighten up and hold tension in this lengthened position to accommodate the shortened hip flexors on the front of your body.
Another example is when the lateral hip muscles (like the gluteus medius and tensor fascia latae, or TFL) are stronger on one side of the body versus the other. With every single step you take, these muscles engage to help stabilize your pelvis. Let’s imagine that these muscles on the right side of your body are weaker than the left side of your body. When taking a step with your left leg, the muscle will engage properly and keep the pelvis level. However, when stepping with your right leg, the pelvis may be unstable because the muscles aren’t strong enough to perform their function. To prevent the pelvis from laterally tilting, your body will respond by engaging the left quadratus lumborum (QL) muscle more than it normally does.

Injuries can cause trigger points
An acute injury creates damage to the connective tissues around the injured area. As these tissues heal and begin to repair themselves, the muscle fibers may tend to tighten up as the body recovers to protect and stabilize the area following injury. This can lead to muscle knots developing, as well as other joint and soft tissue restrictions, which must be addressed even after the injury has “healed” in order to restore your full range of motion.
If left unaddressed, movement pattern compensations begin to occur in order to work around those limitations that came about from the past injuries. Over time, this ultimately affects proper body mechanics and can lead to the development of muscle imbalances (and therefore more trigger points).
Improper body mechanics can cause trigger points
Whether you are working out, doing yard work, or picking up your kids, having the ability to control your body with good mechanics allows you to perform your daily activities in the safest and most efficient way possible.
If your body mechanics are negatively impacted — by an injury, a muscle imbalance, or simply a lack of strength & control relative to the task at hand — then the work being performed by your body is no longer being distributed as efficiently as possible, increasing the risk for injury (and potentially trigger points).
Repetitive movements can cause trigger points
Doing the same thing over and over again utilizes the same muscles (and therefore doesn’t use other muscles), which can lead to the development of trigger points from overuse and other muscle imbalances in the body.
Take a golfer, for example. On a daily basis, they may take hundreds of swings — each of which is performed in the same direction and uses the body unevenly. The hips and thoracic spine will rotate differently, and the glutes and core repeatedly engage more on one side. Now scale the number of swings out to a weekly, monthly, and yearly basis or even out as far back as the person started playing golf — that’s a lot of reps in the same direction!
Stress can cause trigger points
Common reactions to mentally or emotionally stressful situations include the tensing up and clenching your muscles. Coupled with shallow breathing and triggering more of a “fight or flight” sympathetic nervous system response, this may be a recipe for muscle knots to form in the body.
Poor nutrition or hydration can cause trigger points
To perform your daily tasks, your muscles require a certain amount of water and macro/micro nutrients to fuel their performance and also adequately recover. Without a proper recovery, the muscles will not be able to perform at their best and the likelihood of developing trigger points may increase as a result.
How do trigger points affect the function of a muscle?
The muscles in your body need to be able to contract (shorten) and relax (lengthen) on either side of the joints needed to create movement and perform your daily tasks. The presence of myofascial trigger points affects the ability of your muscles to function at their best.
When there are these hypercontracted areas within the muscle, there is decreased blood and nerve supply to the tissue, affecting the muscle to where it no longer performs optimally. If you’ve been working seven days a week without a vacation for ten years, you won’t want to do any more work. Same goes for your muscles with knots in them. And their co-workers (the muscle fibers that are not knotted) end up doing more of the work with less resources. The results may include reduced range of motion, decreased force output, longer recovery times, and increased chances of pain and injuries.
In addition to the impact on your muscles, trigger points can affect how your nervous system perceives the pain. The chemical environment around the areas where your muscles have trigger points changes, where it causes pain receptors to fire more frequently and more easily than in healthy muscle tissue.
The longer that someone remains “stuck” in this environment, the more sensitive their nervous system becomes to feeling pain. This can contribute to more chronic myofascial pain patterns that may later develop into conditions such as myofascial pain syndrome of fibromyalgia.
How to get rid of trigger points
This is the moment you’ve been waiting for! By now, you’ve probably realized you have a trigger point or three affecting your movement and comfort, or sitting quietly to the side waiting to cause trouble. If you are experiencing pain from trigger points, it might be a good idea to begin taking actions to improve and get rid of those tight spots to prevent the pain from getting worse. Depending on your personal preference, you may look to address your trigger points through a self-care approach or see a healthcare professional for treatment.

Could Digestive Issues and Low Back Pain be Caused by Tight Hip Flexors?
Many people act as though health issues are specific and isolated. It’s time for a new angle. The systems in your body are intricately connected: if you’re experiencing problems in one area it can directly affect another.
This domino effect is especially prevalent when it comes to your back, hips, and digestive system.
Your abdominal region is packed full of tissues and necessary systems that you use 24/7. It is home to your bladder, kidneys, female reproductive system and can also be ground zero for potential dysfunction, from ovarian cysts to irritable bowel syndrome (IBS).
Many of these internal organs in your abdomen are also adjacent to the iliopsoas or hip flexor muscles. That’s why it isn’t uncommon for patients to ask me: can IBS cause hip and groin pain?
I’m going to walk you through the inner workings of your abdominal region so you can better understand your body and how your organ health directly relates to your muscle health.
How body alignment and tight muscles affect digestion and back pain
Body alignment is an essential part of overall bodily functioning and health. When your spine or hips are out of alignment, it can throw many things off. And if left unaddressed, it can lead to more complicated medical issues.
The impact of your muscles on your body alignment is also often overlooked. If your muscles – especially your iliopsoas muscles – are too tight, they can pull and shift joint and bone alignment. This misalignment, in turn, can disrupt even your organ function.
The role of your iliopsoas muscle
Your iliopsoas is one of your primary hip flexor muscles. It is comprised of two muscles: the iliacus and the psoas. Your iliacus attaches directly to the pelvis, while your psoas attaches to your lower spine and travels diagonally through your body to where both muscles cross the hip joint and attach to the femur (thigh bone).
The location and overlap from the lower to the upper body are essentially what makes up your body’s core. The iliopsoas acts as a stabilizer for your hips and your spine, so if those muscles are too tight or not working properly, it impacts everything around them.
When your core is weak, your body as a whole becomes weak and wobbly.
Your core helps you perform many daily functions like sitting, standing, squatting, etc. It is no wonder then that your iliopsoas muscles may get tight from all this use; they are continually being used and engaged, and very rarely getting time to relax.
On top of this, the iliopsoas muscles are located right next to your reproductive organs, bowel, bladder, and large intestine. The proximity of the iliopsoas to these systems affords the muscles more opportunities to protect the abdominal organs when one system is struggling or weak.
One primary example is if you have irritable bowel syndrome or any other digestive tract issue.
Your body will react by tightening surrounding muscles to protect that part of your body. Since the iliopsoas muscle is one of the closest muscles to your intestines, keeping the iliopsoas muscle tight is your body’s natural response.
Depending on the location of the organ issue, different parts of the iliopsoas will tighten, and other muscles may also join in. The tension can continue to spread over time or as the condition worsens, causing pain.
Pain from abdominal issues
Now you should have a good understanding of how your muscles, organs, and bones are interconnected and can affect each other when one isn’t functioning properly. You’ve also seen that your body alignment can get disrupted if your muscles are too tight. When your body alignment is disrupted, there is increased potential for organ discomfort or abdominal issues to arise as well.
How tight hip flexors affect the digestive system
Tight hip flexors can affect your digestive health. Your iliacus and psoas are located right next to the small and large intestine. When you begin to have issues with either part of the intestine, it can cause the iliopsoas muscles to quickly tighten around the intestinal area.
Medical issues like irritable bowel syndrome can cause hip and groin pain, which is why if you start to have lower back pain, it could be due to your digestive issues.
As the iliopsoas tightens, it doesn’t much matter where the tightening begins. Once one part of the hip flexor muscles are impacted, the rest of them play an internal tug of war to try to balance and stabilize the core of your body. As the muscle tightness increases, the pull on your bones also increases. This pull is what impacts body alignment and how your joints fit together. These subtle changes can affect your posture, the way you walk, and cause back and hip pain over time.

How tight hip flexors affect the reproductive system and urinary tract
Just as the digestive system can impact muscle health, the reproductive organs and urinary tract are part of your abdominal health as well. Issues with your kidney, bladder, or reproductive organs (ovaries, uterus, prostate) can affect body alignment and iliopsoas tightness.
When your body is going through significant change or trauma, this muscle reaction becomes even more elaborate. For instance, when a woman experiences pregnancy and childbirth, there are some major adjustments her body must make. This additional trauma often causes the iliopsoas muscles to overtighten: they’re attempting to stabilize and realign the hips and back.
Other major organ traumas like ovarian cysts can cause issues with the iliopsoas muscles. The ovaries are very close to the iliopsoas muscle, so once they’re inflamed, the muscle contracts and tightens to keep the area safe and protected.
If you are unsure if you have ovary issues, but you are having groin or abdominal pain, it is important to note muscle tightness. Tight iliopsoas muscles alone can cause groin and abdominal pain, so pain may not necessarily be attributed to the organ itself.
Muscle release for abdominal pain
When you’re experiencing medical issues such as IBS, ovarian cysts, or general digestive problems, working closely with a medical professional is important. There are many contributing factors to your organs’ health, including your diet, exercise routine, and overall wellness.
Tight muscles can also be a major contributing factor to your lower back, groin, and hip pain. With that in mind, finding ways to integrate some muscle-specific exercises, stretches, and releases into your routine could improve your abdominal health and realign your body to get things back on track a bit faster.
Targeted iliacus and psoas release
One of the most effective ways to release tight muscles is to apply prolonged (30-90 second) pressure.
One major issue with the psoas and the iliacus muscle is that they are difficult to reach unless you have a massage therapist or physical therapist there to help you. This is why I invented the Hip Hook.
The Hip Hook is the world’s first muscle release tool for both the psoas and the iliacus. Its unique angled design allows you to apply prolonged pressure while relaxing the rest of your body. Initially, the pressure is applied to the psoas muscle. Pressing down on the handle allows the tip to pivot and apply direct angular pressure to the iliacus. Releasing your psoas and iliacus muscles once a day for just a few minutes can bring astounding results, and you will be able to feel an immediate difference in your hip alignment.
Don’t ignore your backside! Because tight hip flexors affect the front and back of the body, it’s also important to release the muscles in the back of the hips. To tackle those points, you can use the Hip Release Ball.

Abdominal stretches
No matter your condition, adding a bit of stretching into your life will do you good. You should err on the side of caution, however, because too much stretching can be detrimental to your hip flexor muscles. It is best to stretch your iliopsoas muscles in moderation.
Beyond focusing solely on your hip flexor muscles, adding in some trunk twists and back stretches can also be helpful. This spreads out the muscle area being stretched and opens more areas along your spine, hips, and core.
Taking a few gentle yoga or restorative yoga classes can be helpful to give you a few ideas for specific hip or back openers as well as some twists to work into your stretching routine.
Muscle relaxation
Muscle relaxation and muscle release go hand in hand. Since your iliopsoas muscles are engaged continuously even when performing simple tasks (like sitting), they hardly ever get a break from contracting.
Something we often don’t get enough of these days is rest and relaxation. This can come in many forms, but find 10-20 minutes every day to truly relax (and not just right before bed).
Relaxation could be something as simple as lying on the floor and taking deep breaths for 10 minutes. It could be a hip flexor release with your legs resting on the couch while your back is on the floor. It could be scheduling a Swedish massage once a month.
Whatever you can fit into your schedule and budget, I highly recommend taking the time to truly relax your mind and your muscles each day.
Chiropractic care
The final piece of the puzzle that we have for you today is to look after your bones and joints. Many chiropractic doctors and massage therapists will work together to create a healing space for your body.
Chiropractic care may not need to be an ongoing piece of your treatment plan, but if your iliopsoas muscle tightness has pulled your hips or spine out of alignment, then a few visits could be helpful.
As you work to release and relax your muscles, your body will start to realign naturally. However, depending on the severity of the misalignment, you may need some extra help from a chiropractor.
Take control of your abdominal health
The more you understand your body’s inner mechanics, the more you learn how interconnected your organs, muscles, and bones are, the more likely you’ll discover a treatment plan that is right for your body.
To further your knowledge of how the iliopsoas muscle impacts most aspects of your body, check out my book Tight Hip, Twisted Core: The Key to Unresolved Pain.
This book not only contains helpful information on the way your muscles, organs, and bones work together to form a healthy, balanced core, but also targeted stretches and tools to relieve lower back and hip pain.
FAQs on digestive issues
Can tight hip flexors cause digestive problems?
The iliopsoas muscles are in close proximity to the intestines. Tension in the psoas and iliacus muscles can create a general alignment imbalance, affecting the functioning of these organs.
Can tight hip flexors cause constipation?
Muscular tension can compress and restrict organ functioning and bowel movements. Releasing the muscles in this area, especially the psoas and iliacus muscles can provide relief.

Pelvic Pain Causes: from Appendicitis to Muscle Tightness
Pelvic pain can manifest itself in many ways. It comes on very suddenly for some and can cause a range of other symptoms beyond just discomfort.
Pinpointing what causes pelvic pain can be tricky, though, because several medical conditions could be the culprit. What’s more, if your pain is chronic, multiple conditions could be pelvic pain causes.
With so many different systems interacting with the body’s pelvic region, it can be difficult to pinpoint the exact pelvic pain causes right away. This is especially true since when one area of the body begins to malfunction, others tend to follow suit.
Recognizing that you have pelvic pain is usually relatively easy, but figuring out the pelvic pain causes is far more complicated. However, issues related to your pelvic floor and muscle tightness in your iliopsoas often appear together.
While pelvic pain causes can range from digestive issues to the reproductive and urinary systems, the iliopsoas muscles are intimately connected to the other functioning parts of the pelvic floor.
If something is amiss in your pelvic area, the iliopsoas muscles attempt to rebalance and assist the pelvic bone. Unfortunately, this usually causes more harm than good.
What defines pelvic pain?
Pelvic pain is most often defined or described as pain below the belly button (in the anterior lower abdomen). While pelvic pain causes vary, it remains an increasingly common problem among both men and women. However, it tends to be an issue more widespread amongst women.
The origin and intensity of pelvic pain tends to fluctuate from person to person, and no specific disease has been pinpointed to cause it. Depending on the pelvic pain causes, the pain can be categorized as either being acute or chronic.
Acute pelvic pain means that the pain is felt very suddenly and is often very severe or debilitating. Whereas chronic pelvic pain means the pain may come and go, but it could also be constant – lasting for six months or longer.
Common pelvic pain symptoms
The most common symptom of pelvic pain is, of course, pain in your lower abdomen below your belly button. However, how many doctors end up diagnosing pelvic pain causes by looking at other symptoms associated with when the pain began to occur.
When monitoring the severity of your pelvic pain and how long it is present, look for these specific symptoms as well:
- Cramping
- Localized pelvic pain
- Sudden onset of pain
- Pain aggravated by movement
- Pain involving your entire abdomen
- Pain that slowly develops
If you start to develop some of these symptoms, then it is a good idea to start asking, answering, and recording the answers to the following questions. When you visit the doctor for a diagnosis of your pain, you will have a better foundation for them to work from.
- Is the pain dull or sharp?
- How long does the pain last?
- Is anything triggering the pain, or under what circumstances does the pain happen?
- Is the pain occurring during a menstrual cycle, sex, or urination?
- Does the pain begin suddenly or gradually?
- Does the pain come and go?
- How long have you been experiencing any amount of pelvic pain?
When describing your pelvic pain and other symptoms, being as thorough as possible can help your medical provider understand more about your condition and the possible pelvic pain causes.
Pelvic pain causes
As mentioned before, there are two different types of pelvic pain: acute and chronic. Their differences are primarily in how the pain presents – and how long the pain lasts – but the pelvic pain causes can differ.
There can be an overlap between the two types of pain and the underlying causes, so it is essential to weigh all possible options.
Common acute pelvic pain causes
Ovarian cyst
When a fluid-filled sac develops on the ovary, this is called an ovarian cyst. Ovarian cysts are relatively common, and in most cases, will subside without any symptoms. While many go away naturally within a few months without treatment, it can cause pain in the pelvis when the cyst or fluid-filled sac bursts. Pain can also occur in the pelvis if the cyst twists in any way.
Urinary tract infection
A urinary tract infection (UTI) often comes with some form of acute pelvic pain, but it should subside once the infection has gone away. The UTI can present anywhere within the urinary system, including the bladder, urethra, or kidneys.
The severity of the pelvic pain associated with the infection depends on the person and where the infection is located in the urinary tract. However, most pelvic pain will be present when urinating.
Appendicitis
Appendicitis is a painful swelling, usually originating in the middle of your abdomen, that is coming from your appendix. At first, pain may come and go but will increase in intensity as the swelling worsens.
The appendix is connected to the large intestine, and when appendicitis occurs it can put pressure on the pelvis, causing pain. Most pain will present in the lower right-hand portion of the abdomen, and some acute pelvic pain may be present.
Constipation
Constipation, a bowel obstruction, or a bowel spasm can also cause pelvic pain. Common symptoms associated with constipation or bowel obstruction are abdominal pain and abdominal swelling.
Swelling in this lower section of the abdomen puts immense pressure on all surrounding organs and body parts, including the pelvic region. With the increased pressure and abdominal pain, some pelvic pain is possible with severe constipation or an occasional bowel spasm.
Acute pelvic inflammatory disease
Pelvic inflammatory disease can be both acute or chronic. It is usually a bacterial infection of the womb, ovaries, or fallopian tubes when it is acute. In most cases, the infection occurs after an additional infection of chlamydia or gonorrhea, which should be treated with antibiotics. Most localized infections like this cause inflammation, which then causes localized pelvic pain.
Peritonitis
The peritoneum is a thin layer of tissue that lines the abdomen’s interior, liver, kidney, bowel, and other organs in the abdomen. When this tissue becomes inflamed, it is known as peritonitis.
Peritonitis causes sudden and severe abdominal pain that requires immediate medical attention because inflammation of the peritoneum usually means the tissue is infected. Depending on the area, this infection may cause pelvic pain that subsides after the infection has been treated.
Pelvic abscess
An abscess is a collection of pus that can develop anywhere in the body. Abscesses are usually quite painful and are caused by a bacterial infection. A pelvic abscess is the collection of painful pus between the womb and vagina. These abscesses require immediate medical attention.
Pregnancy
Pelvic pain can occur during pregnancy for some women. This type of pelvic pain can be considered acute because it is associated with a temporary condition. However, it does have its own medical term: pregnancy-related pelvic girdle pain (PGP). There can be a more specific diagnosis of symphysis pubis dysfunction (SPD), but that is less common.
PGP is caused by your pelvic joints’ stiffness, or sometimes the joints moving unevenly at the back or front of the pelvis. Both cause pelvic pain.
Common chronic pelvic pain causes
Endometriosis
Endometriosis can also cause acute pelvic pain, but it is far more commonly associated with chronic pelvic pain because it is a long term condition. Endometriosis is a condition that occurs when small parts of the womb lining exist on the outside of the womb. This could be on the ovaries, and when that is the case, it causes extremely painful periods and pelvic pain.
Chronic pelvic inflammatory disease
As mentioned before, pelvic inflammatory disease can be either acute or chronic. The origins of both are the same, and it is a bacterial infection in the womb, ovaries, or fallopian tubes. The main difference is that when you have chronic pelvic inflammatory disease, you will also likely have chronic pelvic pain associated with it.
Irritable bowel syndrome
Irritable Bowel Syndrome (IBS) is a condition that affects the digestive system, causing bloating, cramps, diarrhea, and constipation. Symptoms associated with IBS will come and go with time and vary in severity.
For some people, symptoms could last for weeks or even months at a time. IBS’s exact cause is not yet determined, but for most people, it is a lifelong condition. Due to the intense abdominal pain and associated swelling, chronic pelvic pain is possible, especially during IBS flare-ups.
Inflammatory bowel disease
Similar to IBS, inflammatory bowel disease (IBD) groups two chronic conditions into one umbrella term: ulcerative colitis and Crohn’s disease. Both of these conditions affect the gut in several ways but also can cause inflammation and pelvic pain.
Fibroids
One of the less common chronic pelvic pain causes is developing fibroids or non-cancerous tumors that grow in and around the womb. Most women that have fibroids are unaware entirely, as the fibroids do not cause any symptoms. However, the tumors made up of muscle and fibrous tissue can twist or deteriorate with time. These complications have been known to cause pain, especially pelvic pain.
Trapped or damaged nerves
Many nerves surround the pelvic floor, and if they become trapped or damaged in any way, specific movements or activities can cause pelvic pain. Depending on the type of nerve damage, it could cause a sharp, stabbing, or aching pain that is usually localized to one area of the pelvis. Nerve damages or trappings are also often associated with tight hip flexor muscles due to the additional stress on the pelvis caused by the muscle pull.
Pelvic pain and muscle tightness
Pelvic pain and pelvic pain causes are different for everyone, but when one portion of the pelvic region is unstable, your hip flexor muscles will attempt to correct the issue.
In fact, in some cases, the iliacus muscle could actually be causing the pelvic pain.
Since the iliacus muscles lie on the pelvic bone’s inside surface, they are intimately involved in all pelvic movements and the general well-being of muscles and nerves associated with the pelvic floor.
The primary job of the iliacus muscle is to stabilize the hip and pelvic bones. When pelvic issues arise, the iliacus muscle tightens to protect and stabilize the pelvic area. While the iliacus muscle tightness could simply be a symptom, tight hip flexor muscles can also be one of the pelvic pain causes.
Many medical practitioners that look at the tightness of the iliopsoas in relation to pelvic pain often ask if the muscle tightening is the cause or a side effect of a different condition. In either case, tight iliopsoas muscles could be contributing to your pelvic pain.
Relieve pelvic pain with muscle release
Since muscle tightness seems to be associated with most types of chronic pelvic pain, whether it be a cause or a side effect, finding relief takes a bit of work. You may start to see a physical therapist to understand the root of the pain or find ways to stretch, relax, and release muscle tension.
Although stretching and relaxing your iliopsoas muscles can help, the most effective treatment for tight iliopsoas muscles is to use prolonged pressure to release the tension. To do this, use a targeted tool like the Hip Hook for a few minutes each day.
The Hip Hook is the only tool specially designed to target iliacus muscle tension at the source. Its unique angles design allows the tool to first release the psoas, then pivot to access the iliacus, reaching the inside of the hip bone and allowing the user to relax their body into the Hip Hook while releasing these key muscles.
Depending on the pelvic pain cause you are experiencing, a Hip Hook can be the ideal tool to help get you back on track to recovery quickly. Whatever your pelvic pain causes, releasing tight iliopsoas muscles can help relieve pelvic pain, whether acute to chronic.
FAQs on pelvic pain
Why are my pelvic muscles so tight?
The iliopsoas muscle is involved in everything from sitting to standing, bending to running. They are constantly active. They also tend to tighten to guard other injuries and issues in the pelvic area. Once the iliopsoas muscles accumulate tension, they often don’t release without manual pressure.
How do you release pelvic muscle tension?
Prolonged pressure is the most effective way to release these deeper muscles. It is difficult to access both the psoas and iliacus muscles, because the iliacus is attached to the pelvic bone and it takes a specific angle and depth to reach it. Skilled therapists use their hands to manually release these muscles for their clients, or you can use a tool specific to the job, like the Hip Hook
How do tight hip flexors affect pelvic pain?
The psoas muscle, and more specifically the iliacus muscle, are primary hip stabilizers. When there is dysfunction in the pelvic area, these muscles will tighten to protect the area. When these muscles are holding tension, they bring the entire region out of alignment, creating inefficient movement, twisting, and pain.

Everything You Need to Know About the Sacroiliac Joints and Sacroiliac Joint Pain
The sacroiliac joint (or SI joint) is a very important area of the body (located in the lower back) that is susceptible to pain and injury. It is estimated that up to 25% of cases of lower back pain may be caused from a problematic SI joint.
In this blog, you’ll learn everything you need to know about the sacroiliac joints and SI joint pain (also referred to as SI joint dysfunction), its common symptoms, and what you can start doing today to reduce pain.
- What are the sacroiliac joints? What do they do?
- What are some symptoms of sacroiliac joint pain?
- What are some causes of sacroiliac joint pain?
- Three muscles that affect sacroiliac joint pain
- Three ways to improve your sacroiliac joint pain
What are the sacroiliac joints? What do they do?
If you were to place your hands at the base of your lower back, you’d likely feel two “bumps” on the back side of your pelvis. Sometimes also referred to as “dimples” in your lower back, this is where your sacrum connects to the ilium bones and forms the sacroiliac joints. There are many soft tissues (muscles, ligaments, cartilage) that hold the SI joints in alignment and support the small, yet very important, movement that occurs in this joint with every single step that you take.
The SI joints provide stability in the body, helping to support your body weight and distribute external forces (e.g. lifting, picking up your kids) evenly across the pelvis to reduce pressure placed on the lumbar spine. They also absorb shock and impact (e.g. playing sports, stepping off of the sidewalk, landing each step during a run), helping to efficiently transfer energy between the lower and upper halves of the body.

What are some symptoms of sacroiliac joint pain?
The symptoms of sacroiliac joint pain may vary slightly from person to person.
The pain is often felt in the lower back and upper buttocks region, the immediate area around the SI joint. Some people describe the pain in this location as being dull and achy, while others may experience more of a stabbing, sharp pain in the lower back.
Other symptoms of sacroiliac joint pain include radiating pain down into the hips, groin, and back of the upper thigh. Additional feelings of tightness, stiffness, burning, tingling, numbness, or weakness may be present and describe some of the sensations felt on the painful side.
Certain activities or body movements typically performed on a daily basis may become more challenging and also increase the symptoms. Examples include: twisting or leaning back towards one side; lying down or sleeping on the affected side; going up and down stairs; stepping off of the sidewalk; and sitting, driving, standing, or walking for too long.
What are some causes of sacroiliac joint pain?
Common causes of sacroiliac joint pain include (but are not limited to) misalignment of the pelvis, traumatic events or past injuries, pregnancy, hypermobility, sports, and more. We’ll share our view on each of these potential causes in more detail below.
Misalignment of the pelvis (pelvic torsion and anterior pelvic tilt) can cause SI joint pain
Pelvic torsion is where one side of the pelvis rotates forward into an anterior position relative to the other side, creating a twist in the pelvis. This rotation changes the orientation of the sacrum and ilium bones, affecting the way that they move relative to each other. As these structures begin to rub each other the wrong way, the soft tissues of the SI joint wear away and become irritated over time.

Why is my pelvis twisted?
This misalignment happens as the result of muscle imbalances that develop and hold the pelvis in this off-balanced position, such as a tighter iliopsoas on one side. The iliopsoas is your body’s main hip flexor, consisting of both the psoas muscle and the often overlooked iliacus muscle — which you will learn more about as you keep reading.
A rotated pelvis is also a common contributor to other conditions, such as scoliosis, leg length discrepancy, and many single-sided pains in the body. Don’t blame these other “diagnoses” as the root cause of your sacroiliac joint pain. It all stems from the rotated pelvis caused by muscle imbalances around your hips.
Anterior pelvic tilt is a misalignment of the pelvis where both sides of the pelvis rotate forward into an anterior position, creating an excessive arch in the lower back. Some strain is placed on the SI joints in this position, with a lot more force being placed on the joints of the lumbar spine.
SI joint pain caused by traumatic events or past injuries
Traumatic events, such as a car accident or falling on your tailbone, can force the pelvis out of alignment and cause pain in the SI joints. Similarly, past injuries (or surgeries) to the foot, ankle, knee, or hip can lead to compensations in the way you move your body. Over time, this creates muscle imbalances (which we talked about above) that work their way up towards the pelvis, impacting its alignment and also the way movement occurs in the sacroiliac joints.
SI joint pain after pregnancy
A recent survey of 1,000 women found that a significant majority of them were unaware that sacroiliac joint pain is one of the leading causes of lower back pain in women 35 years and older who have been pregnant in the past.
When a woman is pregnant, a hormone called relaxin is released into the body. As you may have guessed by the name, this hormone helps the muscles and ligaments in the woman’s pelvis to relax. This supports a growing fetus and also allows for more laxity and expansion in the joints of the pelvis for the child to pass through the birth canal during delivery.
As amazing as pregnancy and childbirth can be, these events can later lead to developing sacroiliac joint pain. While the relaxin helps make childbirth possible, it also has the effect of increasing the instability of the woman’s pelvis (which is a naturally stable area of the body). Because relaxation of the pelvic joint ligaments (which include both the SI joints and the pubic symphysis) creates additional stretch and movement, the surrounding muscles and ligaments hold tension in an effort to create stability in those joints to protect the body.
There may even be pre-existing muscle imbalances or asymmetries in sacroiliac joint laxity on either side of the pelvis before the pregnancy, which later contributes to developing pain in the SI joint during and/or after pregnancy as the surrounding muscles and ligaments experience stress and hold tension.
SI joint pain caused by hypermobility
People who are hypermobile, or those who participate in sports and activities such as gymnastics or yoga, tend to have “looser” joints. Think about someone who can perform the splits. While they can move into a larger range of motion than the average person, the joints in their body are typically less stable. To protect the body, the brain sends signals to the surrounding muscles to hold tension to help stabilize the joints in these extended positions. This tension can compress the SI joint and contribute to muscle imbalances where one side of the body has more range of motion than the other.
SI joint pain from golf, baseball, or football
Collision sports (such as football or hockey) and rotational sports (like golf or baseball) can play a role in the development of sacroiliac joint pain in athletes.
Taking a hard hit in football or receiving a hip check in hockey when you are least expecting it can have an impact on the body. A collision such as this can have enough force to knock the structures of the pelvis and the body out of alignment, leading to the athlete experiencing pain in the SI joints.
The demands placed on the body during that of a golf swing or a baseball swing can be significant. There is a certain amount of rotation required to be coming from the hip joints and the thoracic spine during a “perfect” swing in order to protect the joints in the lower back and pelvis. When range of motion in these areas is lacking, movement must be created elsewhere (like in the lumbar spine and SI joints). These areas are meant to be stable, and this increased movement can place a constant shearing force on these joints, leading to pain developing over time after hundreds and thousands of swings irritating those areas.
These are just a few examples; other sports and activities can certainly contribute to developing pain in the sacroiliac joints. Think about what we’ve already talked about above and consider how it applies to the things you do in your life.
Three muscles that affect sacroiliac joint pain
While there are over 40 different muscles in the lower back, hips, and glutes that surround the sacroiliac joints in your body, we believe that the iliacus, piriformis, and quadratus lumborum muscles are among the most important ones for you to focus on first to improve your pain.
How does the iliacus cause SI joint pain?
The iliacus muscle lines the inside surface of the pelvic bone (or ilium) and connects to the iliac crest and iliac fossa on the ilium, the top edge of the tailbone (the ala of the sacrum), and the lesser trochanter (the inside of the femur near the groin).

The primary function of the iliacus is to stabilize the hip joint and the sacroiliac joint (or SI joint), keeping those two joints aligned and strong regardless if the body is stationary (such as when sitting or standing) or if the body is moving (such as when walking or running). Other secondary functions of the iliacus include assisting in hip flexion and hip external rotation.
Since the iliacus is active when sitting, standing, walking and running, it is being used constantly throughout the day, increasing the likelihood of this muscle becoming chronically tight. Tightness in the iliacus muscle pulls the pelvic bone forward into an anterior rotation, where the lower back is chronically arched.
This creates strain where the sacrum and ilium meet – the SI joint! The longer these structures are misaligned, the more unhappy they become, and the more likely you’ll develop pain or discomfort in this area.
How does the piriformis cause SI joint pain?
The piriformis muscle connects to the sacrum, the ilium, and the greater trochanter on the femur. Its primary functions include assisting with external rotation and abduction of the hip, as well as stabilizing the hip inside of the hip socket.
When the piriformis becomes tight, it pulls on the sacrum and ilium and can lead to compression or misalignment about the SI joint. As you continue to move your body with these supporting muscles not functioning optimally, the sacrum and ilium rub each other the wrong way and cause the soft tissues inside the joint to become irritated.
A tight piriformis muscle often goes hand-in-hand with tight hip flexors, like your iliacus and psoas muscles. This is because your body is searching for balance on each side of the hip. If the hip flexors on the front of the hip are tight and pulling the pelvis into an anterior position, the muscles on the back side of the hip (like the piriformis) will tighten up and play a game of tug-of-war. This combination of a tight iliacus and tight piriformis is very common among people who are experiencing SI joint pain.
How does the quadratus lumborum cause SI joint pain?
The quadratus lumborum muscle (or the QL muscle for short) attaches to the bottom of the 12th rib and the transverse processes of the L1-L4 vertebrae and connects to the iliac crest (of the ilium) and also the iliolumbar ligament, which helps to stabilize the sacrum and the sacroiliac joints.
The quadratus lumborum muscles function together to help extend the lumbar spine, and they can also function unilaterally to side bend the spine. With its connection to the bottom rib, the QL also functions to stabilize the diaphragm when you inhale with each breath.
A tight quadratus lumborum muscle pulls on the ilium and iliolumbar ligament that it attaches to. This may result in a rotation of the pelvis or a hip hike on one side of the pelvis, changing the alignment between the ilium and sacrum. As we’ve discussed with the other muscles, this ultimately affects the movement of the SI joints and can lead to pain.
Three ways to improve your sacroiliac joint pain
The key takeaway here as it relates to keeping your SI joints happy and healthy revolves around good alignment. Throughout the course of our lives, there are so many things that contribute to the development of muscle imbalances that pull us out of alignment and cause pain.
You absolutely must take care of the muscles that support the movement of the pelvis so that the ilium, sacrum, and other structures can move efficiently and work together as they were designed to do. The pelvis is part of the “core” of your body, and when it is well-supported and in good alignment, the rest of the body works better.
Do these 3 things to improve SI joint pain
1) Release the tight muscles surrounding your pelvis.
We already talked about 3 muscles that may be tight and contributing to your sacroiliac joint pain. Explore each of those muscles with muscle release techniques and stretches to reduce tension and tightness that has built up in them, likely over YEARS.
The piriformis and quadratus lumborum muscles can each be easily accessed by a massage therapy ball or lacrosse ball (or similar), as these muscles are more superficial. However, the iliacus muscle, one of your body’s main hip flexors (along with the psoas muscle), is a little bit different and is not easily accessed by a ball to truly get the right amount of pressure and precision needed for an effective release. For this, you need to see a manual practitioner or have a special tool that can do the job.
My favorite muscle release tool for the iliacus muscle is the Hip Hook. The Hip Hook was invented by Christine Koth, MPT, who was a physical therapist for 20+ years and noticed a common theme among the patients she worked with – tight hip flexors! When the hip flexors get tight, they can cause pelvis alignment issues and create tons of problems throughout the body.
The Hip Hook is designed to get into the hard-to-reach psoas and iliacus muscles (your body’s main hip flexors) to relieve tension, increase range of motion, and decrease pain. Other tools and therapy balls simply don’t address BOTH of these muscles, which may be key to long-term pain relief and improvement.

2) Strengthen the muscles surrounding your pelvis to improve muscle imbalances.
Reducing tension and tightness with muscle release work and stretching alone may not fully address the “root cause” of your sacroiliac joint pain. It is likely that these muscles are compensating and trying to perform the work done by other, larger muscles that have weakened (perhaps from too much sitting, inactivity, past injuries, etc.).
Some of these areas that often become weak on people (and maybe on you too) include the glutes, hamstrings, core, and smaller hip stabilizers around the pelvis. Try waking them up with some of these hip strengthening exercises and see how your body feels.

3) Work on exercises specific to improving your hip mobility.
Adding direct hip mobility exercises into your routine is another way that you can strengthen the muscles that support the movement of your hips and improve the active range of motion through which you can control your hip joints. This is not to be confused with stretching, which simply takes the hip through its passive range of motion.
These can be some really amazing hip mobility exercises that you can try to start improving how well your hips move, helping to keep your pelvis aligned in better position, and reducing the pain that your SI joints may feel.
Looking to learn more about your body?
You’ll get answers to your questions about tight hip flexors and learn how they can affect the functioning of your entire body. Discover the “3 Simple Steps” to realigning your pelvis and improving the way your body feels in the book “Tight Hip, Twisted Core – The Key To Unresolved Pain” by Christine Koth, MPT.
Frequently asked questions about sacroiliac joint pain
What do the sacroiliac joints do?
The SI joints provide stability in the body, helping to support your bodyweight and distribute external forces evenly across the pelvis to reduce pressure placed on the lumbar spine. They also absorb shock and impact, helping to efficiently transfer energy between the lower and upper halves of the body.
What causes sacroiliac joint pain?
Sacroiliac joint pain can be caused by several different factors, including (but not limited to) misalignment of the pelvis, traumatic events or past injuries that resulted in compensations, pregnancy, hypermobility, and sports.
How do I relieve sacroiliac joint pain?
Relieving sacroiliac joint pain centers around being able to improve the way the pelvis is aligned, which in turn helps the sacrum and ilium move better together and reduce pain. This can be achieved through a combination of muscle release and strengthening, stretching, and mobility exercises that address currently existing muscle imbalances around the hips and pelvis.

Three Steps to Reduce Lower Back Pain During Pregnancy
There is no dancing around the fact that motherhood can be painful. It is a beautiful and rewarding journey, but a woman’s body goes through some significant changes and traumas during the pregnancy and birthing process.
Having back pain during pregnancy is almost an expectation for most women. The thing is, that lower back pain from pregnancy often sticks around for months, and sometimes years, after your baby is born.
But it doesn’t have to.
The hip flexor muscles are major players in the anatomical changes a woman’s body goes through during and after pregnancy. Because of their deep connection to the hip and pelvis, it is not uncommon for tight muscles to become even tighter with the strain of carrying a baby.
The best way to avoid lower back or sacroiliac joint pain during pregnancy is to get ahead of it, especially since it is widely known as an issue for pregnant women.
Understanding how your body changes as your baby grows, during birth, and beyond will set the stage for three ways you can prevent or manage lower back pain from pregnancy.
Tailbone and lower back pain during pregnancy and beyond
The lower back pain that you experience during pregnancy can start before you even are pregnant, and can continue long after you’ve given birth.
Before pregnancy
The way your hips are aligned before you even get pregnant will influence if you have lower back pain during pregnancy – and how severe it is if you do.
The hip flexor muscles, or iliopsoas, take on the brunt of supporting the pelvis as it changes during pregnancy. So whether you have flexible hip flexors or tight hip flexors, even before you get pregnant, will impact how your body adapts and reacts during pregnancy.
Having relaxed hip flexors before pregnancy often means that your pelvis and hips are properly aligned, and will be fully prepared to handle the variety of physical changes that occur during pregnancy and birth.
Hypermobility also impacts many women and can mean your hip flexors are too relaxed to fully stabilize and support hip movement. A balance of strength and flexibility is necessary to prevent lower back pain in pregnancy.
During pregnancy
If there are underlying issues with your hip flexors before you get pregnant, that’s when you run into issues with sacroiliac and lower back pain during pregnancy. This is not just because your hip flexors were too tight to begin with; it’s also because your body is changing to prepare for giving birth.
One of the most prevalent changes that occurs during pregnancy is that your body releases a chemical hormone called relaxin. This hormone relaxes (hence the name) the ligaments in the pelvis and softens connective tissues surrounding the cervix.
The reason the body does this is to ensure your baby can easily leave the birth canal. Essentially, relaxin is your body’s natural way of creating elasticity and space for the baby during childbirth.
Obviously, loosening everything up for childbirth is extremely important, and you want that to happen. But ligaments are the fibrous tissue that connects bone to bone and stabilizes, in this case, the pelvis. The loosening of these ligaments that hold the hip and pelvis together is part of the reason why so many women experience back, tailbone, or hip pain during and after pregnancy.
The instability of the iliopsoas muscles and the continued release of relaxin hormones contributes to muscle tightness. It seems counterintuitive for your body to tighten muscles when relaxin is being released. But as the ligaments and other tissues loosen, your iliopsoas tightens to try to stabilize the pelvic region.
Women that have a genetic predisposition to extra elastin, or are naturally hypermobile, will experience even looser joints during pregnancy and, in turn, even tighter hip flexor muscles. This can lead to lower back pain in pregnancy.
Post pregnancy
As natural a giving birth may be, your body still experiences it as trauma. Your baby’s position, and the birthing position itself, puts your iliopsoas muscles into an extremely strained position.
During childbirth, the body will be hypermobile in the pelvic region regardless of your pre-pregnancy hip flexors. So for any woman, the iliopsoas is working hard to keep the pelvis stable during the birthing process.
Since the iliopsoas is strained and shortening during birth, it is normal for women to have hip and lower back pain post-pregnancy. Many women expect this pain to subside as their pelvis heals and returns to normal, but the issue is that once the iliopsoas has tightened, it doesn’t easily relax again on its own.
This continued muscle tightness is why many moms, even years after giving birth, continue to have the same sacroiliac and lower back pain after pregnancy as they did during it.
How your muscles can cause back pain
It can be hard to imagine that muscle tightness causes your sacroiliac pain or lower back pain during pregnancy. The fact is: From walking to sitting to running, the iliopsoas muscles (the primary hip flexors) are involved. They are engaged during almost every bodily movement that you make.
When the iliopsoas muscles are too tight, your joints and bones are pulled out of alignment. This in turn leads to more issues and pain over time.
The iliopsoas muscle is made up of two muscles: the psoas and the iliacus. The psoas originates at the vertebrae of your lower spine, and the iliacus originates on the inside of your pelvic bowl. The muscles both cross the hip joint and attach to the top of your femur (the thigh bone). Both the spine and the pelvis are responsible for lower back and sacroiliac joint alignment.
This relationship of the iliopsoas to these integral bone structures and joints means that when there is trauma or stress around the pelvis, the iliopsoas muscles step in to protect it. Their primary job is to stabilize, so if there is an irritant threatening to cause your hip region instability, they tighten to reinforce balance.
However, this also happens in reverse. When your hip flexor muscles start too tight, they can cause trauma or stress in that area. It is a domino effect: If one aspect is out of whack, it creates issues elsewhere. That’s why you experience lower back pain during pregnancy in addition to other bodily traumas.
So what can you do about your lower back pain during pregnancy? There are three helpful steps to releasing your tight hip flexor muscles, but you must be proactive if you want to enjoy the benefits of all three of them.
Three steps to healthy hip flexors
Working through all three steps to release your hip flexor muscle tightness and relieve back pain will only be possible before or after pregnancy. There are some ways to release the front of the hip during pregnancy, but they will not be as consistent or easily accessible.
1. Releasing the front of the hip
Releasing the front of the hip is by far the most difficult – and one of the most vital – aspects of improving your iliopsoas muscle health.
To do this, you need to reach the iliacus and the psoas muscles, which is tricky because the best release point is tucked slightly behind the hip bone. To reach this area, you need a physical therapist to help you or a tool like the Hip Hook.
Unlike other massage tools, the Hip Hook is specifically designed to access both the psoas and the iliacus muscle. The unique shape allows it to reach around the hip bone and press directly onto the iliacus muscle, providing a much-needed release.
Releasing both the psoas and iliacus are essential to healthy hip flexors. If you have really tight hip flexors, you can also use a tool like the Hip Release Ball. The size, shape, and density of the ball are perfect for releasing the front psoas muscle.
These tools cannot be used during pregnancy. Getting this muscle released isn’t impossible though. You may be able to work directly with a physical therapist to relieve your lower back pain during pregnancy, as they will know how to release the muscles in a way that will not be harmful.
If you are trying to get pregnant, it can help to start this three-step process before conception. This will prepare your body for all of the hormonal changes that influence lower back pain during pregnancy.
Once you’ve given birth and have had ample time to heal, you should begin with this front hip release once again.
As mentioned before, after the trauma of giving birth, your hip flexor muscles will have tightened even more. So, your lower back pain after pregnancy may be even worse than during pregnancy. Regular hip flexor release will help establish alignment and relax the muscles.
2. Releasing the back of the hip
Since the muscles in our bodies work in tandem, you need to balance things out and release the back of your hip as well. The Hip Release Ball mentioned in the last section is the perfect tool to do this.
Although you will not be releasing your iliopsoas muscle when lying on your back, you will want to release your piriformis muscle. This muscle is often related to sacroiliac joint pain and sciatica; learning to access and release this muscle during pregnancy can be a complete game-changer during pregnancy.
When your iliopsoas muscle is tight, it will pull on various parts of your body, including the piriformis muscle. If the piriformis muscle is tight, it will pull on the iliopsoas muscle. This tug of war will continue unless they are both released.
To do this, lay on your back and place the Hip Flexor Release Ball under your glute, near the center of one buttcheek. When you find a tight spot, relax into that; you want to put prolonged pressure on these spots for 30-90 seconds to help them release. Do this on both sides of your hip.
During most of your pregnancy, you should be able to release the back of the hip, which will relieve some of your lower back pain during pregnancy.
3. Realignment exercises
The last step in this process is to perform realignment exercises. These exercises can be done (and are effective) before, during, and after pregnancy. Once your hip flexor muscles are being released with the tools described above, begin integrating realignment exercise into the routine.
When your iliopsoas muscles are tight, they often will pull the hips, back, and tailbone out of alignment. So, helping your body realign during this three-step process will only have benefits for your body.
To enable you to do this even during pregnancy, you can do the exercise either on your back, standing, or seated.
Before you start, note that this exercise is only meant to be performed on one hip, unlike the muscle releases. So, you will need to decide which side of your body has the tightest iliacus muscle. The reason behind this is because the tightest side of your body is going to be pulling your hip forward slightly, causing misalignment.
You can watch this hip realignment exercise, but to give you an idea of what to expect, I will explain how the realignment exercise works when lying on your back:
- Lie down on your back
- Bring both knees up towards your chest so your feet are off of the ground
- Place a hand behind the knee on the designated side of your that is tighter and being pulled forward
- Squeeze your hand behind the calf by bending your knee
- Simultaneously push against your hand without moving, as if you are trying to push your foot towards the ground
- Naturally, your hand will resist this pressure. You don’t need to press too hard, so only apply a mild/moderate amount of force.
- The opposing leg will simply stay up off the ground during this time so it doesn’t accidentally push into the ground.
- You will hold this pushing motion with your hand for two seconds, or one deep breath
- Then, relax for a few moments
- Repeat 10 times
If you’d like to learn more about how to realign your hips properly and complete the three-step process, my book Tight Hip, Twisted Core breaks it down in detail, along with providing other necessary information about how tight iliopsoas muscles can impact your life – and how releasing them can free you from your lower back pain during pregnancy.
FAQs on lower back pain during pregnancy
Why does lower pain back occur during pregnancy?
Part of the problem includes tension in the hip flexors, which tighten to provide stability in the pelvis.
Is it normal to have lower back pain in pregnancy?
A pregnant body is changing daily, and the muscles and ligaments of the body are constantly compensating for the needs of the growing baby as well as preparing the body for childbirth. This creates stress and tension in different parts of the pelvis, and can often be relieved by releasing the tight muscles.
How can I relieve lower back pain in pregnancy?
Follow a three-step system: release the front of the hip, release the back of the hip, and realign the pelvis to release muscle tension. Releasing the front of the hip will require the help of a skilled practitioner if you’re pregnant, but you can still get relief by following the last two steps.

Torn Hip Labrum Symptoms: Finding the Cause of your Hip Pain
Hip pain and hip injuries can manifest in many ways. If you’re experiencing pain in your hips, it can often be difficult to know the root cause.
One of these causes may be a hip labrum tear.
A hip labrum tear might not always hurt at first, but over time you may start to notice a few differences in your hip mobility and ability to perform specific movements.
When you’re experiencing hip pain, you may be looking to find the one culprit – the too-soft mattress, the heavy grocery bags, the extra 50-miles on your bike. It’s important to remember that your hip structure is complex and has many moving parts that work together to create smooth, pain-free movement.
Understanding what your hip labrum is, where it is located, and what causes the labrum to become damaged over time is just as important as knowing how to treat it. You can then use this information to incorporate preventative care could help you avoid a hip labrum tear altogether. Or to help you spot potential hip labrum tear symptoms early on.
What and where is the labrum of the hip?
The hip labrum is a disc of cartilage that is strong and flexible enough to allow for the fluid movement of your hip joint. This durable cartilage rims the outer socket of your hip joint, deepening the joint surface and allowing for a wider range of motion. It also keeps the joint fluid in place. When the joint fluid is in the joint capsule, it reduces friction.
The hip labrum is located between the socket and the ball of your hip joint. It should cover the entirety of the ball and socket connection points on both hips, though everyone’s body is a little different. It then sits between these two bones to avoid direct contact with each other and protect them from friction when you are moving.
Beyond protecting the hip joint itself, the labrum helps to keep the ball and socket in correct alignment. You can think of your hip labrum cartilage as being like a rubber gasket. It keeps the joint’s ball and socket in place, and prevents damage during all of your movements.
What are torn hip labrum symptoms?
Recognizing that you have a torn labrum can be difficult because hip labrum tear symptoms can present similarly to hip arthritis pain symptoms.
If you suspect you have a torn labrum, or even if you’ve just strained it, your iliacus muscle will likely be tight. And it’s the pain from this muscle – or the sensation of tight hips – that might be your first indication of a bigger problem in your hip joint.
Your iliacus muscle is one of the two muscles that make up your hip flexors. Paired with the psoas, the muscles are known as the iliopsoas. Together, the iliopsoas muscles are what bring movement and stability to your hips, thigh bones, and pelvic bone. They allow you to make everyday movements like going from standing to sitting position, or lifting your knee up to your chest.
Another job of the iliopsoas muscles is to stabilize your core and protect the ligaments and bones in your hip joints. Therefore, the muscles may contract or overcompensate when there is a problem, such as increased friction, misalignment, or a labral tear, causing increased tightness and pain in your hip flexors.
Still, in many instances, those that have experienced such a tear may not actually experience torn hip labrum symptoms or pain. It may take time for the pain to manifest in the hip, as the iliopsoas muscles attempt to correct the injury on their own.
Although you might not have all (or any) of the most common symptoms of a labral tear, they could present as one or more of the following:
- Limited hip mobility and range of motion
- Pain in the hip (usually the groin area) that worsens with extended periods of staying in the same position
- Sensations like clicking, locking, or a feeling of catching when moving the hip joint
The way hip labrum tear symptoms present can also depend on the type of labral tear it is: anterior or posterior.
Anterior labral tears are by far the most common type of labrum tear. Located in the front of the hip, this part of the labrum is thought to be easier to injure because of the lack of blood vessels in that area.
Posterior labral tears are less common than anterior tears partially because they are located on the back of the hip. While this joint area still moves frequently, there isn’t as much motion creating contact on the labrum cartilage in the back as there is in the front.
If a posterior labral tear occurs, it is because more stress is occurring in the back portion of the hip joint. This could be from frequently performing a repetitive motion like frequently squatting with weights or partaking in other squatting and lunging sports.
If you begin to experience these symptoms during activities that normally don’t cause pain or discomfort, it is time to seek the help of a professional.
Diagnosing a hip labrum tear
As we mentioned, you may not always know you have a torn hip labrum. Symptoms are not always identifiable. But getting a proper diagnosis of any hip injury is important to ensure that you get the appropriate treatment.
In most cases, a physical diagnosis will include a variety of orthopedic tests, communication about your medical history, a rundown of your current fitness routine, a history of your past injuries (if any), and a general physical assessment.
It’s important to share all this because labrum tears are common with serious athletes that use their hip joints repetitively and aggressively. Participating in sports like dance, gymnastics, hockey, or soccer requires very specific hip movements and rotations. This can put extra stress and pressure on the hip joint itself, as well as extra strain on your iliopsoas muscles.
These labral tears can also be caused by hip joint abnormalities, such as hip dysplasia. The way your ball and socket fit together could result in added friction or pressure in specific areas, leading to damage and tears later in life.
Doctors and physical therapists alike will test for a labral tear in much the same way. During a physical examination, they will measure joint strength, flexibility, and range of motion. They’ll be checking to see if there is any obvious swelling and listen to your feedback about which movements are causing pain in your hip flexors, legs, lower back, and pelvic region.
If there is obvious pain for the patient when testing for these things, it can be a strong indication that the ball and socket of the joint are not adequately protected.
A standard test that doctors use to determine whether a labrum tear has occurred or not is called the FABER test. FABER stands for flexion, abduction, and external rotation. This specific test puts the hip joint into a position to expose anterior labral tears.
The FABER test works by having you lay on your back with straight legs. Then, you put one leg in a figure-4 position.
Your physical therapist or doctor will gently apply pressure to the knee of the bent leg. If there is groin pain on the side of the bent leg, it could be a hip labrum tear symptom. It is an indicator that there is a problem in your hip muscles, such as your iliopsoas muscles, or that there could be a joint injury.
Hip labrum physical therapy and other treatment options
Once you have identified torn hip labrum symptoms – and determined that your hip pain is indeed being caused by a torn hip labrum – now is the time to address it.
Repairing cartilage is a difficult task for the body, but it is not impossible.
The most common treatments for hip labrum tears include injections, anti-inflammatories, rest, and physical therapy. I always recommend that you begin with the least invasive treatment, opting for natural solutions such as rest and physical therapy that focuses on releasing and stabilizing your iliopsoas muscles. Only if those are unsuccessful should you move on to more aggressive treatments.
Anesthetic fluid injections
Depending on the severity of your pain and the other torn hip labrum symptoms you’re experiencing, a doctor may recommend an anesthetic fluid injection for pain management.
By mitigating some pain, you can integrate other movements and physical therapy.
However, this type of intra-articular injection is most often recommended if the pain and other hip labrum tear symptoms cannot be alleviated by a different treatment measure.
Non-steroidal anti-inflammatory drugs
Another common treatment is the use of anti-inflammatory medication, generally non-steroidal, to help control your hip labrum tear symptoms. Like the injection, this is meant to mitigate pain to allow for continued treatment of other kinds as opposed to being a complete solution in itself.
These non-steroidal anti-inflammatory drugs should also bring down the swelling caused by the friction and irritation of the damaged hip joint.
Rest and recovery
One of the best treatments for doing away with hip labrum tear symptoms is simply to rest for a while. This can be hard to do if you are an athlete, but giving your body time to heal is essential.
In most cases, though, this doesn’t mean all activities have to halt.
Many patients who experience hip labrum tear symptoms are only recommended to stay away from painful activities. So, if running is causing you pain, but walking isn’t, a doctor may recommend that you stop running for a short period of time to let the labrum rest and avoid pain.
You should also be incorporating very light stretches or movements designed specifically to release your hip muscles, which may reduce or eliminate hip flexor pain and restore natural alignment in your hips and pelvis.
Hip labrum exercises and physical therapy
Working closely with a physical therapist is a great treatment option for almost any type of hip pain, especially a labrum tear. A physical therapist can come up with individualized treatment plans that will help you to improve strength and stability in your hip joints.
Many physical therapists focus strictly on labrum hip tear exercises that help you build up the muscles surrounding your hips like the iliopsoas muscles, glutes, abdominals, and back muscles. Improving muscle strength in these areas is a proven way to help stabilize the hip joint and protect it from future damage.
The hip flexor and hip labrum injury
When a part of the hip structure is damaged, especially a part so integral to movement like the labrum, your muscles tend to try and pick up the slack and support the hip more intensely. With hip labrum tears, we often see this happening with the iliopsoas or hip flexor muscles.
Since the hip flexors engage with nearly every hip movement, it makes sense that a tight hip flexor often correlates with a labrum tear. Keep in mind that this can be both a torn hip labrum symptom, and a cause of a labrum tear.
A tight iliacus muscle can begin to pull your hip out of alignment, which directly opposes what the labrum does. One of the labrum’s jobs is to keep your hip joint aligned and in place.
So, with the extra pull of each movement, your labrum will be experiencing far more pressure than usual. Over time, this can lead to the cartilage wearing down and eventually tearing.
On the other hand, if you’ve experienced a trauma of some kind that tore your labrum, you may not notice any hip labrum tear symptoms until the iliopsoas muscle tightens more. This occurs because the iliopsoas is compensating for an imbalance of some kind in the joint structure.
Whatever the cause of the muscle tightness, one thing is for sure, if you have a hip labrum tear, more often than not, your hip flexors will be tight too.
And, to find long-lasting pain relief, you need to make sure to release your hip flexors.
Hip labrum pain relief by releasing the iliopsoas
Knowing your hip anatomy and how your body is meant to work together in unison makes it easier to understand where your hip pain is coming from. Living with and treating a hip labrum tear comes with many symptoms that often disguise themselves as arthritis or other issues.
Once you’ve been diagnosed, and treatment begins, it can be helpful to start looking at other contributing factors, such as your tight iliopsoas muscles.
Treating the iliopsoas muscles is two-part. There is the psoas, which can be massaged along the connecting point of your inner thigh and pelvis. But the iliacus muscles can be relatively difficult to release. It connects to the internal side of your hip bone and requires a precise angle and amount of applied pressure. Therefore, it is nearly impossible to reach with an average massage ball, foam roller, or your own fingers.
A skilled physical therapist is trained on iliacus muscle release, but you can’t do this effectively alone between sessions or as a preventative measure.
There is one self-massage option, though. The Hip Hook by Aletha is the only tool designed to reach the precise point where your iliacus connects to your pelvic bone, using body weight to apply the right amount of pressure.
It’s safe to use as a part of your daily routine. And, as your iliopsoas loosens, you’ll likely experience less pain, less tightness in your hip flexors, and less stress will be put on the cartilage of your hip joints.
Once you have rebalanced your hip joints, strengthened them through physical therapy, and given your hips the rest they need, any hip labrum tear symptoms you have been experiencing should decrease and may even disappear. And if you feel that familiar hip flexor tightness or hip pain start to flare up, you can easily use your Hip Hook at home.
If you’d like more information on targeted hip stretches and exercises, or would simply like a deeper understanding of your hip labrum, iliopsoas muscles, and the many other components of your hip joints, check out my book: Tight Hip, Twisted Core.
Armed with all your new knowledge, you’ll surely be able to kick your hip labrum tear symptoms to the curb.
Frequently asked questions about a torn hip labrum
What are common symptoms of a torn hip labrum?
Common symptoms of a torn hip labrum include: limited mobility and pain-free range of motion in the hip joint; pain in the hip or groin area that typically worsens with extended periods of inactivity; and sensations like clicking, locking, or a feeling of catching when moving the hip joint through certain ranges of motion.

Ultimate Guide to the Iliopsoas: What it does, why it hurts, and what to do about it
Your iliopsoas muscles are part of your hip flexors: when they are tight, you might experience lower back, hip, knee, or even foot pain. Learn how to lengthen and strengthen your psoas and ilThe iliopsoas is composed of two muscles that together connect your upper half to your lower half, provide stability for your entire lower body, and are chronically underappreciated.
You may not have spent much time thinking about your deeper core muscles – you can’t see or easily touch them, so they stay out of sight and out of mind.
We take a different angle: we know, from decades of experience, that tension in these deeper muscles is the root cause for many unresolved pains in the hip, back, knee, and even feet.
If these deeper muscles of your body are tight or imbalanced, it affects your entire body. Just because you can’t see them in the mirror doesn’t mean they aren’t playing a major role in your mobility, your strength, and your aches and pains.
Anatomy of the Iliopsoas
Let’s start by looking at all the parts, like an IKEA furniture diagram.

The bones and joints around the iliopsoas muscles
- Hip Joint: The hip joint is a ball and socket joint, formed between the pelvis and the head of the femur.
- Femur: The femur is the thigh bone, also the longest and strongest bone in the body.
- SI Joints: The SI joints are located between the iliac bones and the sacrum, connecting the spine to the hips.
- Lumbar Vertebrae: The lumbar vertebrae are the bones that make up the spine below the cervical and thoracic vertebrae, but above the sacrum/pelvis.
- Ilium: Ilium is made up of two large bones forming each half of the pelvis, after you take out the sacrum.
There are 2 main iliopsoas muscles
You have two iliopsoas muscles that originate on either side of your pelvis and low back. And each of the iliopsoas muscles are actually made up of two muscles: the psoas and the iliacus. They have different starting places, but both end at the top of the thigh bone (femur), like the letter “Y”.
One part of this muscle – the psoas– travels from your lower back, across the front of your pelvis, and attaches to the femur (thigh bone). Too often, we think of ourselves like paper dolls with a front side and a back side. But you’re 3-dimensional! This muscle crosses diagonally through your body in a direction we rarely think about.
The other part of this muscle (the iliacus) travels from the Iliac fossa (the pelvic bone) and crosses over the hip joint (directly affecting the SI joint) to attach to the femur. Take a Deep Dive into the Anatomy of the Hip Flexors here.
What does the iliopsoas do?
Short Answer: Stability and hip flexion.
Both muscles are responsible for general stability and for hip flexion (lifting the knee, as in marching or going up stairs). Due to its insertion to the spine (low back), the psoas is also responsible for arching your lower back. Picture the inside prong of the ‘Y’ as the psoas, and the outer prong the iliacus. Because of these insertion points, they pull on the thigh bone differently. A tight psoas will pull your low back towards your knee. A tight iliacus will externally rotate your thigh bone, resulting in your foot turning outward.
The psoas and the iliacus both contribute to hip flexion motion, but their primary job is to hold together the hip, pelvis, and lower back area.
What does the iliacus do?
Short answer: it’s the glue that holds your hip joint, SI joint, and femur together.
Primarily, the iliacus stabilizes the hip joint and the SI (sacroiliac) joint. Because it is relatively short and strong and crosses the two joints of the hip as well as the sacroiliac joint, it acts as more of a stabilizer. The iliacus keeps those two joints aligned and strong regardless of whether the body is stationary or moving. Long muscles have good lever arms for moving bones well. A good example of a long muscle is the quadricep, it goes from the hip to below the knee. Short muscles are built to hold parts in place. The iliacus, being more of a short muscle, was born to stabilize the hip and SI joint. Any situation that challenges these two joints will lead to a challenge to the iliacus muscle and possibly the development of chronic tightness.

Ever have a loose thread? What happens when you give it a tug? Usually, everything that attaches to that thread starts to get pulled along with it. You can think of the iliacus this way: if it’s tight, it’s going to pull the body into misalignment.

What does the psoas do?
Short answer: it connects the upper body to the lower body.
The psoas stabilizes the hip and SI joints just like the iliacus, but it is also responsible for the stability of the lumbar spine and flexion of the hip joint.
Similar to the iliacus, the psoas stabilizes the hip and SI joint, due to its connection to the lumbar spine. In addition, its close connection to the lumbar vertebrae and its attachment to the front and back of each vertebrae allow it to hold the lumbar spine in place. When there is any issue in the low back, the psoas grabs on for dear life to hold it all together, easily developing into chronic tightness. Its complex attachments at the lumbar spine also contribute to motion of the spine such as rotation, side bending, flexion and extension, but primarily its job at the lumbar spine is to stabilize.
Why do I have tight hip flexors? Why do my hip flexors hurt?
Happy muscles don’t hurt and short and knotted muscles are not happy.
The cause of tight hip flexors may vary: Perhaps you sit a lot, or you habitually cross the same leg over the other. Maybe you have to drive often and hover your foot over the pedal more than most. Maybe you played rotary sports like baseball, golf, or hockey that have you twisting primarily in one direction. Maybe your work from home (or work-from-couch) set-up is less than ideal, or your body is protecting past injuries. Any one of these can cause a contracted iliopsoas muscle. Most of us have more than one of these causes, making a perfect storm.
What can I do about my tight hip flexors?
Stopping the muscle contraction is the first step.
When we say contraction, we mean shortening (and not the buttery kind). Muscles can contract as a whole or only part of the muscle can contract creating what we refer to as a muscle knot. Bring your palm to your forehead; you just shortened your bicep. Now hold that position for at least 8 hours, 7-days a week, and you will have recreated the problem with the iliopsoas. When you sit for eight hours a day, you are contracting (shortening) the iliopsoas. Do this long enough, and the muscle gets stuck trying to hold this position, so that when you stand up or lay down, this muscle is trying to yank you back into that seated position. It’s not worth getting frustrated with the iliopsoas; it’s just trying to help you, and it needs some TLC and attention to relax.
The first steps to relaxing your hip flexors
Relax, then lengthen.
If you notice, we keep saying contracted and using (shortened) in parentheses. This is deliberate. Most practitioners (physios, chiropractors, personal trainers) will tell you to stretch a tight muscle. Which would make sense if it was short, but stretching isn’t enough if it’s short AND stuck in a contracted state.
You’ll need to stop the contraction before you can lengthen the muscle
When any part of your iliopsoas is contracted, stretching it is like walking up to a terrified person in the fetal position and trying to pry them out of it. A better tactic is to calm them down, rub their shoulders, and remind them to take deep breaths. That’s exactly the first step in releasing the iliopsoas.
How to release the iliopsoas
The best way to release the iliopsoas is by prolonged pressure: muscles relax first through pressure, then stretching.
Muscle tissue is smart, and the fascia – the connective tissue that surrounds and holds every organ, blood vessel, bone, nerve fiber and muscle in place – is even smarter. Muscles and fascia both have sensors called mechanoreceptors which means our tissue can sense even the slightest change in temperature, pressure, vibration, even noise. Think of these sensors as two fire alarms: the stretch and pressure alarms. If two alarms are going off and you only silence one, are you going to be able to relax? Probably not.
Why is pressure on the iliopsoas important?
Pressure helps to relax the muscle and surrounding connective tissue, and provide immediate relief, calming the area down. The tissue’s mechanoreceptors will send signals to the brain that it can relax and stop holding tension in the area. Only then can you begin to correct the issue with stretching and realignment exercises. If you jump right into stretching, you trigger only one of the receptors; by tomorrow you may be back where you started. This is why so many people are stuck on the stretching hamster wheel: the tightness builds back up, so they have to go stretch it out again. The missing ingredient for most tight psoas and tight iliacus muscles is prolonged pressure, best delivered through a massage or using a massage tool.
How to apply pressure to the iliopsoas
You can’t just dig into this area all willy-nilly. Not to mention how uncomfortable that would be, this area is crowded with organs, arteries, and nerves. This is a case of “location, location, location”. If you spend the time finding the tight spots in your psoas and iliacus, you will know how to release your own iliopsoas. And it’s so worth it.
There are many ways to access the psoas for psoas release. Some people prefer their physical therapists get in there manually, the DIYers may prefer a lacrosse ball (although that ball is too small), or a Hip Release Ball if you have a very tight psoas. Because the psoas is hard to reach and there is no ball or tool that can effectively reach the iliacus, I designed the Hip Hook for all of my suffering clients: the only muscle release tool targeting both the psoas AND the iliacus muscle. The iliacus can only be addressed through specific angular pressure, so finally having a tool that is able to hit those spots is magical.
The Hip Hook is unique because of its angular pressure
Once you have located the sweet spot, you simply lay on the Hip Hook, allowing it to sink into the psoas for 30-90 seconds. Once you have relaxed, it is time to push down on the lever and feel the tip pressing up and into the iliacus muscle, pinning it against the ilium. Apply this prolonged pressure again for 30-90 seconds while breathing and relaxing. While the pressure can feel intense at first, you’ll likely feel a shift and release after 30-60 seconds. Prolonged pressure is important here. You may feel the desire to move around and rub the spot but in the case of muscles holding tension, they don’t like to be rubbed and any benefit you may feel temporarily will be short term.

After releasing the hip flexors, don’t forget your back side
A tight iliopsoas creates misalignment, causing other muscles to work overtime to compensate. You’ll want to apply pressure to these muscles as well (plus, it feels SO good). This is where the Hip Release Ball comes in handy. Because the glutes, piriformis, and QL (quadratus lumborum) muscles are easier to reach and respond to perpendicular pressure, you don’t need an advanced tool to release them. A simple ball or even foam roller will do the trick if you know what you’re doing. (If you don’t, please check out this video on how to release the back of the hip after you have released the iliopsoas).
How to stretch the iliopsoas
After applying prolonged pressure to the iliopsoas and the posterior (back side) hip muscles, now it’s time to stretch! The lunge stretch is highly recommended because it stretches the iliopsoas, bringing circulation and length to that muscle.
Step one foot forward with your spine straight. You can do this stretch with your knee on or off the ground. With this stretch it’s important to engage your abdominal muscles or contract your glutes to eliminate the forward tilt of the pelvis while tucking your butt under you. This allows for the iliopsoas muscle to stretch fully over the joint while protecting your lower back from the psoas tugging on it while it’s being stretched.
You should feel the stretch in the front of your hip joint or the front of your thigh. If you’re not feeling it there or if you’re feeling it in a different spot, then stop. You can experiment with bending your spine to the opposite side of the leg you’re stretching to increase the psoas stretch.
To get lasting results from your hip flexor stretch, focus on using proper form and take generously deep breaths.
Developing a plan to take care of your tight hip flexors
Prolonged pressure and light stretching is hopefully all you need to find relief. However, if you have experienced this issue for a very long time you may have more work to do. In my book Tight Hip Twisted Core, I lay out the Three Simple Steps to understanding and relieving unresolved pain. If you want to know what caused your hip flexors to tighten in the first place (and take preventative measures) this is a good place to start.
In over 20 years of clinical physical therapy practice, I have seen that nearly every client on my table had some degree of iliacus tightness causing a twisted pelvis and resulting in misalignment throughout the body. Tight iliopsoas muscles are merely a side effect of modern living, and we all need to be masters of this area of our body to be well and strong. I hope this information has set you on your path to being one of a growing number of iliacus and psoas masters.
FAQs about the iliopsoas
What is the function of the iliopsoas?
The function of the iliopsoas is to connect the lower body to the upper body, maintaining stability, facilitating lumbar rotation, lateral flexion and hip flexion. If the iliopsoas is too tight, it can affect the functioning of the entire body.
How do I release the iliopsoas muscle?
The iliopsoas responds to direct and angular pressure, anywhere from 30-90 seconds. It’s a tricky muscle to access, and using a muscle release tool like the Hip Hook is the best way.
How do I stretch the iliopsoas?
A kneeling hip flexor stretch is the simplest way to stretch the iliopsoas and hip flexor complex. But it is most effective when followed by releasing the iliopsoas.

How to Get Lasting Results from a Hip Flexor Stretch
Most people think that simply stretching their hip flexors will solve their pain and tightness. We have a different angle. To get the best and longest-lasting results from a hip flexor stretch, we believe that adding in muscle release techniques, plus strength and mobility exercises, will take your routine to the next level.
Why do I have tight hip flexors?
It is extremely common to have tight hip flexors.
Take a moment to think about how much time you spend sitting down each day, on average. Between working at your desk, studying or attending class, driving your car, relaxing at home on the couch, eating meals, you can see how the hours add up quickly. And that’s just for one day!
Despite the health risks for sedentary behavior, many people spend up to 70% of their waking hours in a seated position each day. Here’s the math: that equates to about 11 hours of sitting each day (assuming that you sleep 8 hours each night).
Throw in the additional stay-at-home restrictions that many of us have experienced this year related to COVID-19, and the amount of time we spend sitting and not moving our bodies each day has further increased.
Sitting shortens our hip flexor muscles relative to their natural length when we are standing. When stuck in this shortened position for extended periods of time, the likelihood of developing tight hip flexors increases, especially as you repeat this pattern day after day.
Additionally, there are many other activities that we do on a daily basis that may contribute to tight hip flexors. When we walk or go for a run, our hip flexors are constantly being used to move one leg in front of the other. These muscles are very active when we are working out, helping to stabilize the low back and hips when doing exercises like squats, deadlifts, and lunges. Many sports involve a lot of hip flexion, such as cycling, kickboxing, and gymnastics.
Taking all of this into account, you can see how overworked your hip flexors may be and why it is so important to take care of these muscles with some TLC.
How can tight hip flexors impact the body?
Tight hip flexors can have a big impact on how the ENTIRE body functions.
Let’s begin to paint the picture by talking about the pelvis, the core, and how a tight hip flexor affects the way these structures of the body are aligned.
The pelvis is situated at the center of the body, making up a very important piece of your core. Yes, we are referring to the same “core” that many people assume simply consists of the abdominal muscles. Your core consists of much more than that!
Think of your core as a 3-D box with 6 sides:
- Front – rectus abdominis and transverse abdominals
- Back – spinal erectors, quadratus lumborum (QL), and other back muscles
- Sides – internal obliques and external obliques
- Top – diaphragm
- Bottom – pelvic floor muscles
The pelvis is a very important piece within this 3-D box, connecting the upper and lower body together. Looking deeper inside of the core and pelvis, there are two very important muscles that play a big role in supporting your body’s alignment – the iliacus and the psoas.

As depicted in the image, tightness and imbalances in the iliacus and psoas muscles twists the pelvis and twists the core. Due to its connection with the upper and lower body, this has a chain reaction effect above and below.
The pelvis connects to the spine, which twists and affects the alignment of the rib cage, shoulders, and neck. The pelvis also connects to the hips, where the way the femur moves within the hip socket is changed and affects the ways the knees, feet, and ankles work.
Now that you’re aware of the potential effects that tight hip flexors can have on your body, here are some helpful tips to keep your hip flexors (and the rest of your entire body) as happy as possible so your whole body can feel good.
Tips for getting the best hip flexor stretch
1. Gain an understanding of what the different hip flexor muscles are and where they are located.
Without first having a general understanding of which muscles in your body are hip flexors and where they are located, it is going to be more challenging to achieve the best hip flexor stretch possible to target the areas that are tightest.
The hip flexor muscle group includes (but is not limited to) the following:
Psoas Major – Connects to the lower thoracic and lumbar vertebrae (T12 through L5) and also to the lesser trochanter (inside of the femur near the groin region).
Iliacus – Runs along the inside surface of the pelvic bone, connecting to the top edge of the tailbone (at the SI joint) and also to the lesser trochanter.
NOTE: The psoas major and the iliacus muscles both cross the hip joint, where they join together and form what is known as the iliopsoas tendon.
Rectus Femoris – Also part of the quadriceps muscle group, this muscle connects to the anterior inferior iliac spine (lower part on the pelvic bone, or ilium), just above the acetabulum (hip socket), as well as down the leg where the quadriceps tendon inserts into the base of the patella (kneecap).
Tensor Fascia Latae (or TFL) – Connects to the anterior superior iliac spine (ASIS) and also the deep fascia of the iliotibial band (IT band). This muscle is right about where your pants pocket would be if you were wearing a pair of athletic shorts.
Pectineus – Connects to the pubic bone and the inside of the femur (thigh bone).
.jpg)
[Read More from Aletha: Deep Dive into the Anatomy of the Hip Flexor Muscles]
2. Pick an appropriate hip flexor stretch to effectively target the correct muscle.
There are many different stretches for tight hip flexors to choose from. So how do you know which one is the right one for you?
With your new understanding of the different muscles that make up the hip flexor muscle group and where they are located in the body, you may begin to see how you’ll need to perform stretches that target your tight hip flexors from multiple angles.
This helps you to focus on stretching each individual hip flexor muscle and give them the specific attention that each may need. This will be up to you to explore what your own body needs and determine which of these will be the best hip flexor stretches to help you achieve the results you are looking for.
[Read More from Aletha: The Best Hip Flexor Stretches for Tight Hips]
3. Perform the hip flexor stretches with proper form and technique.
After you’ve picked the best hip flexor stretch needed to target the right muscle in your body, it is time to get down onto the floor or on your yoga mat to perform the exercise.
The effectiveness of the hip flexor stretch is largely affected by using proper form and technique, which includes a focus on taking nice, big, deep breaths. This really helps to target the correct muscles and help the body relax, where the brain sends signals to the targeted tissues to let go of tension and lengthen.
4. Establish a consistent hip flexor stretching routine and stick to it.
You’ve gained an understanding of your hip flexors. You’ve picked the right stretch to use to target the correct muscle. You’ve performed the hip flexor stretch correctly and remembered to breathe. You are now feeling pretty good. That’s great!
So, what next?
If you’re a fan of feeling great and free of pain, this one time that you stretched likely isn’t going to help you long-term. Instead, setting up a regular routine to do some stretches for tight hip flexors or stretches for the rest of your body is a better idea to help you achieve this goal.
The routine that you set for yourself can be simple and easy. Perhaps you aim for 10-15 minutes of stretching your hip flexors each day (or every other day). You can do multiple sessions per day, splitting the time you stretch between the morning and afternoon. Maybe you even want to stretch out before bed, helping you fall asleep quickly and wake up feeling refreshed.
Routines are great and can help you stay feeling good over a long period of time. Find one that works for you and stick with it. Your hips and your body will thank you for it!
Other tips to make your hip flexor stretches more effective
If stretching your tight hip flexors alone isn’t enough to provide lasting relief or if you are really looking to take your stretching results to the next level, consider these additional tips to include in your routine to see how it makes you feel.
1. Add hip flexor muscle release techniques to your routine.
If your muscles aren’t relieved of tightness after performing your hip flexor stretches, it could be a sign that tension is being held in the muscles in the form of muscle knots. Applying direct and prolonged pressure (for about 30-90 seconds) to these areas first can be more effective at getting the muscle to release tension than simply stretching alone.
If you don’t have the luxury of having a roommate who happens to be a massage therapist or have the ability to see a practitioner in person on a regular basis, using a muscle release tool can be helpful. However, using the right tool for the different muscles to achieve the best results is an important factor to consider.
Muscles like the TFL, rectus femoris, and pectineus are closer to the outside surface of the body, making them much easier to access and target. Using something like a lacrosse ball (or a slightly larger ball) or a foam roller generally works for these muscles.
When looking to apply direct pressure to the deeper hip flexor muscles, like the psoas and the iliacus, the lacrosse ball and foam roller don’t have the ability to get deep enough to access these muscles and also don’t have the precision to target the correct location.
The Hip Hook is a muscle release tool designed specifically to get into the hard-to-reach psoas and iliacus muscles to deliver the best possible release of tension, helping your hips and body feel great.

2. Add muscle activation and strengthening exercises to your routine.
When your muscles and joints feel “tight” it is very common to think that these areas need to be stretched in order to make them better. While stretching may provide some relief in the short-term, these muscles may tighten back up over the next few days.
Why does this happen?
The muscles in your body are meant to control your joints to create movement and also to stabilize your joints to keep them safe. When you sit for longer periods of time, you don’t use or challenge your muscles.
With this inactivity, your hip muscles “turn off” and become weaker. This can then lead the brain to send signals to tighten these muscles up as a form of protection, essentially creating stability by holding tension because the muscles themselves do not have the strength to do so.
The saying “use it or you lose it” is definitely applicable here.
Getting some activation with hip flexor strengthening exercises can help increase the amount of blood flow and activity within the muscles, helping to build strength and increase the effectiveness of your hip flexor stretches over time. Additionally, targeting the other muscles around your hips and the muscles in your core with strength exercises can be a really good idea.
Try some of these hip strengthening exercises out and see how it makes your body feel.
3. Add direct hip mobility training to your routine.
Hip mobility exercises are another way that we can strengthen the hips and improve the active range of motion through which we can control our hip joints. This is not to be confused with stretching, which simply takes the hip through its passive range of motion.
These can be some really amazing hip mobility exercises that you can try to start converting your passive range of motion into an active range of motion, improving the function of your hips and improving the way that you feel.
Want to deepen your knowledge and your stretch?
You’ll get answers to your questions about tight hip flexors, how they affect the functioning of your entire body, and plenty of stretches and exercises to keep you out of trouble in the book “Tight Hip, Twisted Core – The Key To Unresolved Pain” by Christine Koth, MPT.
Frequently asked questions about tight hip flexors
What is the main function of the psoas?
The psoas muscle connects the upper and lower halves of the body. Its main functions are to stabilize the lower back and flex the hip. Other functions of the psoas include external rotation of the hip, as well as extension and lateral flexion of the lumbar spine.