Your cart is currently empty!
Category: Pain

The Best Hip Flexor Stretches for Tight Hips
Are you only stretching one hip flexor? The “hip flexors” are actually a whole group of muscles that help you walk, kick, bend, twist, and stabilize your pelvis. Most people have performed a basic hip flexor stretch at some point in their lives. While it may have led to experiencing some relief, it can be more helpful to use targeted stretches for the muscles that are tight on your body (not your neighbor’s).
In this article, you’ll learn about why the hip flexor muscles become tight and practice several completely manageable hip flexor stretches for even the tightest of hips. These stretches affect your hips from all angles to relieve tightness and keep your whole body feeling strong and limber. One of the best parts about these hip flexor stretches is that the same movement can stretch different muscles, depending on the width of your stance and angle of your body. (So you really only have one stretch taking up valuable memory space.)
[Read more from Aletha: Deep Dive into the Anatomy of the Hip Flexor Muscles]
Why are my hip flexors so tight?
Whether you are someone who is physically active or not, the amount of sitting that the typical person does each day contributes to the development of tight hip flexors. Sitting places the hips into a flexed position, where the psoas muscle, iliacus muscle, and other hip flexor muscles find themselves in a shortened position.
Not only are your hip flexors likely spending longer periods of time in this shortened chair-sitting position (don’t get me started on the couch-sitting position), they also play an important role in helping to stabilize and support your lower back and pelvis in a stable upright posture.
When you throw in the additional demands placed on the hip flexor muscles when walking, running, cycling, working out, picking up kids (and everything they’ve dropped on the floor), and so many other activities we perform on a regular basis, you may begin to see how these very important muscles work overtime for our bodies day after day.
If you don’t take the time to help these muscles lengthen and recover, hip tightness develops over time and it can affect your hips, lower back, knees, and other areas of the body.
You don’t need to stop any of those regular activities (although I’ll evangelize about taking frequent breaks from sitting in front of your computer), but the next time you’re taking a chair-free break from work or getting ready for a workout, give a few of these stretches a try. Your tight hip flexors will thank you for it!
The best stretches for your tight hip flexors
To get the most effective and longest-lasting results from a hip flexor stretch, it’s important to pick the right stretch to target a specific muscle and also perform the stretch with proper technique. Here are several different hip flexor stretches; discover which ones work best for you while learning a little bit about your amazing body. (And if it doesn’t feel amazing right now, check in again afterwards.)
Best stretches for the iliopsoas muscle
The iliopsoas is your main hip flexor and consists of two muscles – the iliacus muscle and the psoas muscle. Depending on your personal preference, you can effectively stretch these hip flexors using a kneeling hip flexor stretch or a standing hip flexor stretch, both of which are described below.
Half-Kneeling Hip Flexor Stretch

- Get down into a half-kneeling position with your front and back knees at about a 90-degree angle. Your stance should be around shoulder-width apart and your pelvis should be facing forward.
- Squeeze the glute on the back leg and also engage your lower abdominals, trying to tuck the pelvis to flatten out your lower back. You may feel a stretch at the front of your hip on the kneeling side.
- Keeping those muscles engaged, gently shift your pelvis forward to increase the stretch.
- With the arm on your kneeling side, reach overhead and across towards the opposite side of your body, allowing your body to side bend slightly to lengthen the psoas muscle.
Standing Hip Flexor Stretch

- Place one foot about 2 feet in front of the other with the feet placed around shoulder-width apart. The front and back knee will have a slight bend in them. Keep your pelvis facing straight ahead.
- Squeeze the glute on your back leg and engage your lower abdominals to try to tuck the pelvis to flatten out your lower back. You may feel a stretch at the front of your hip on the back leg.
- To increase the stretch, gently shift your pelvis forward by pressing your foot into the ground to straighten your back leg. The front knee may bend a little more. Be sure to keep the glute and abs engaged.
- With the arm on the same side as the back leg, reach overhead and across towards the opposite side of your body, allowing your body to side bend slightly to lengthen the psoas muscle.
Best stretches for the TFL muscle and the pectineus muscle
The tensor fascia latae (TFL) is a hip flexor muscle located on the outside of the hip that also connects to the iliotibial band (IT band). The pectineus is a hip flexor muscle located on the inside of the hip in the groin region.
.jpg)
You’ll stretch these muscles using the same instructions as the kneeling and standing hip flexor stretches mentioned above, but will make two slight adjustments to change the angle of the stretch to target the outside of the hip (TFL) or the inside of the hip (pectineus). All of the other instructions remain the same.
To target the TFL muscle, the first adjustment is setting up with a narrower stance, around hip-width apart. The second adjustment is shifting the pelvis diagonally towards the back leg. (Note: you will feel the stretch in the outside of the hip on the back leg).
To target the pectineus muscle, the first adjustment is setting up with a wider stance, slightly outside shoulder-width apart. The second adjustment is shifting the pelvis diagonally towards the front leg. (Note: you will feel the stretch in the inside of the hip on the back leg).
Kneeling, it looks like this:

Standing, it looks like this:

Best stretches for the rectus femoris muscle
The rectus femoris is one of your quadriceps muscles, but is the only one of that muscle group that crosses the hip joint and acts as a hip flexor. The following stretching variations using a kneeling or standing position can effectively target the rectus femoris and the other quadriceps muscles on the front of your thigh.
Couch Stretch

- Get into a half-kneeling position about shoulder-width apart, where the front knee is at about a 90-degree angle. The back knee is bent with your back foot up against a wall, a couch, or being held in position by your hands reaching behind your body.
- Squeeze the glute on the back leg and also engage your lower abdominals, trying to tuck the pelvis to flatten out your lower back. You may feel a stretch at the front of your hip and into the front of the thigh.
- Keeping those muscles engaged, gently shift your pelvis forward to increase the stretch.
To help make it more comfortable on your knee, consider doing this on a softer surface or add a cushion or yoga mat underneath your kneeling side.
Standing Quad Stretch

- From the standing position, reach back to grab your foot or ankle and bring your heel towards your butt. Stand up nice and tall.
- Squeeze the glute on the back leg and also engage your lower abdominals, trying to tuck the pelvis to flatten out your lower back. You may feel a stretch at the front of your hip and into the quads.
While performing this stretch, you can lean up against a wall or hold onto something with your other hand for support. This removes balance from the exercise and allows you to focus entirely on the stretch.
Want to deepen your knowledge and your stretch?
You’ll get answers to your questions about tight hip flexors, how they affect the functioning of your entire body, and plenty of stretches to keep you out of trouble in the book “Tight Hip, Twisted Core – The Key To Unresolved Pain” by Christine Koth, MPT.
Hip flexor stretch FAQs:
What are hip flexors?
The hip flexors are a group of muscles in your body that assist in hip flexion, the movement of bringing the knee closer to the chest. This muscle group includes the iliacus, psoas, rectus femoris, tensor fascia latae, pectineus, sartorius, adductor brevis, adductor longus, adductor magnus, gracilis, and even part of the gluteus medius.
What do hip flexors do?
The hip flexors play an important role in moving your body. Every single time that you take a step, you are using your hip flexors to bring your leg forward. These muscles also help to stabilize and support your hips, pelvis, and spine.
Why are hip flexor stretches important?
Hip flexor stretches are important because they can help increase range of motion in the hip joints, reduce pain and tightness, and improve the way your body performs in your daily activities.
What problems can tight hip flexors cause?
Tight hip flexors can contribute to many different problems throughout the entire body, including hip pain, knee pain, back pain, foot pain, and more.

Are Your Muscles Roadtrip Ready? How to Avoid Hip Pain During a Long Drive
You may love road trips for several reasons, but hip pain probably isn’t one of them. Although you may be mindful and take plenty of breaks to “stretch” your legs while you drive, hip pain while driving is an increasingly common problem, whether it is during your morning commute or cross-country trip.
One thing for sure is that any pain, no matter the cause, should never be ignored. Without proper attention or treatment, hip pain while driving can lead to more issues down the road. Literally.
Just like when you sit all day at the office, if your body is in one position for too long while driving, then two small muscles are taking the brunt of the work.
Those muscles are your hip flexors.
More specifically, they are two connecting muscles: the iliacus and psoas, which together are often referred to as the iliopsoas. And, if you have hip pain while driving or hip pain after a long drive, that pain could be the result of these tight hip flexor muscles.
This article will help you better understand the function of your hip flexor muscles, and how these muscles could be causing you pain while driving. Plus, I’ll give you some tips and tricks to avoid hip pain during and after a long drive.
What causes hip pain while driving?
Although you may feel like sitting is a “resting” position for your body, your iliopsoas muscles are actually engaged the entire time. You see, the iliacus keeps your pelvis stationary and aligned with your thigh bone while your psoas holds your spine straight. They stabilize your entire body and allow you to maintain this position. Essentially, if your iliopsoas stopped working while you were sitting, you wouldn’t be able to sit upright at all.
The problem is, these muscles aren’t meant to be in this seated, shortened position for a long time. Eventually, your iliopsoas muscle gets cramped and starts to develop painful muscle knots. You may feel these in your hips or glutes, but you may also feel them in your lower back on either side of your spine, or even into your thighs. And these parts of your muscle stay contracted even after the rest of your muscle has relaxed.
This muscle shortening and hip pain can happen with any regular sitting positions, but tends to be exacerbated by the limited mobility when driving. Additionally, when driving, your right iliacus and psoas are experiencing even more strain because you’re constantly using your right leg to accelerate and brake. If you have a manual transmission, then both the right and left iliopsoas muscles are being engaged very frequently.
On a long road trip, you may benefit from using cruise control more often, but there will still be some strain on your hip flexor muscles because of your restricted seating position.
On top of all this, when you are on a long drive, it can be difficult to relax because you’re paying attention to the road and other drivers. After all, you need to be alert and able to react if you have to stop or accelerate. This extra tension can fatigue your hip flexors even more, making that tightness and pain even worse.
Unfortunately, hip pain while driving might not be the last of your worries either. Did you know that your tight hip flexors could actually create a whole bunch of other issues for your body?

How hip pain can lead to sciatica, knee, and back pain
A little bit of hip pain while driving might not seem like a big deal at the time. But, if you have noticeable pain and ignore it, it could spread and lead to something worse.
When your hip flexors, especially the iliacus muscles, are allowed to remain tight, it creates a domino effect with neighboring muscles, nerves, and joints.
Even if your pain after a long drive isn’t severe, or it’s simply presenting as some tightness, it could be contributing to other issues that impact your day-to-day quality of life. Sciatica, hip pain while sleeping, knee pain and back pain are all often connected, and it often starts at your hips.
Anytime your iliopsoas is knotted, tight, or contracted, it can pull your pelvic bone forward, throwing your pelvis out of alignment. When you have an anterior-rotated pelvis, it means that one of your pelvic bones, either the right or left, is rotated forward in relation to the opposite side. A rotated pelvis can create problems all the way down to your foot.
When tight hip flexor muscles get to the point of causing alignment issues, more strain is put on surrounding areas. For instance, when one pelvic bone is rotated forward, it puts strain on the tailbone connection, creating pain and tensions where they meet. This can cause sacroiliac pain.
You may feel pain in your hip joint first: when hip alignment is off, there is extra tension being put on the hip socket, and it won’t rotate or move correctly. The now ill-fitting hip socket can cause an internal rotation with your thigh bone, impacting how your leg functions from the hip down. The thigh bone’s internal rotation puts an unnecessary and unnatural strain on your knee because the kneecap doesn’t track normally anymore.
As your lower leg rotates inward, this can also cause your foot to pronate.
As you can see, a little bit of hip pain while driving may seem harmless, but if your iliopsoas is tight enough to impact hip alignment, it more than likely is impacting your knee and foot alignment as well.
Since your psoas is also an integral part of your hip flexor muscle group, it has a similar chain reaction when it is chronically tight. But, in the case of the psoas, this chain reaction moves up your body instead of down.
The psoas muscle connects from the front of your thigh bone to your spine and lower back. While tight psoas muscles can also move down the thigh to impact your lower extremities when tight, they are also likely to pull your spine into an arch, compressing and bending the side of your body that is tight.
As your psoas tightens, it will pull and pull on your spine and irritate the various structures in your lower back. Because the psoas and iliacus work together, the pulling of your iliopsoas can create pelvic rotation and tension that moves from your hips to your feet or your hips up to your shoulders and even your neck.
So, what may have started as just some slight hip pain while driving can cause you to eventually experience sciatica pain while driving, leg pain while driving or many other irritating issues.
Because it all starts with your hips, let’s take a look at some easy ways you may be able to avoid – and relieve – your hip pain while driving.
3 simple ways that could help you avoid hip pain while driving
If you have a long drive or road trip planned, it’s time to take some preventative measures to avoid hip pain while driving. There are only so many things you can do during your actual drive, so the time you spend on your hip health before and after you get in the car is important.
Here are three simple practices you can put in place before your next road trip or long commute:
1. Keep a healthy sitting position while driving
As I mentioned before, sitting for prolonged periods will always result in the shortening of the hip flexors. Still, there are some sitting positions that are worse for your hips than others. So let’s learn a thing or two about good posture for preventing hip pain while sitting in your car for periods of time.
First, do your best to sit as upright as you can. This may be hard in your car because of how the seats are constructed, but if you can, engage your lumbar support in your seat and put the seat back up. This is so when you are resting your back on the seat, your body is supported in the upright position.
Overall, you want to avoid slouching, even if it feels more comfortable in the moment. Try to find a seating position that allows your knees to be slightly past 90 degrees, and your feet to rest on the floor.
You should be able to reach the pedals without having to straighten your leg completely. A slight tilt forward can bring your hips above your knees, taking some strain off your iliopsoas muscles and reducing hip pain before and after you sit in your car.
So, before your trip, take some time to move your seat around and find the perfect position to support your hip flexor health.
2. Take breaks to stretch and move your hips
If you can, take breaks throughout your drive to walk around and stretch. Make use of the rest stops by adding a few extra minutes to do a deep lunge stretch or back stretch, a few hip flexor stretches, and to take a walk.
If you plan a long lunch break and it is a nice day, you can also choose to have an outdoor picnic, pack a yoga mat, and do a few more stretches before driving again.
Whenever you stop driving that day, you may be tempted to rush into your destination and collapse because you’re tired.
But it’s important to take a moment to stretch and move your hips before sitting down or lying on the bed. This will help you alter the shortening of your hip muscles and encourage other types of movement or engagement.
3. Relax and release hip flexor muscles after driving
Since your hip flexor muscles are engaged the entire time you are driving, one of the best things you can do post-road trip is take 10-15 minutes to relax your muscles.
The hip flexor muscles are difficult to relax because they are engaged when sitting and laying down.
One good way to relax the iliopsoas muscles is to find an ottoman or couch, lay on the floor with your butt up against the base of the furniture, and rest your lower legs and feet on top of it.
In this position, your legs should be at a 90-degree angle. With your calves and feet resting on the ottoman, you should have a chance to relax. This position will take strain and tension off of your iliopsoas muscles.
After you’ve given your hip flexors time to recoup in the resting position, then we hope that you packed a few helpful muscle release tools on your trip.
Especially if you have chronic hip pain, I always encourage people to make room in their luggage for muscle release and massage tools. After all, your body is going through atypical stress and will need a little extra love.
Packing a Hip Hook and Hip Release Ball will give you the relief you need to be prepared for another day of driving on your road trip – and enjoying your destination once you arrive!
The Hip Hook is a simple, compact hip flexor release tool that targets the source of your hip pain: muscle tension. By applying direct, prolonged pressure to the iliopsoas muscles, you can release trigger points and knots after a long drive.
The Hip Release Ball allows you to more gently release the psoas muscle and also address muscles like the piriformis on the back of your hip structure.
Remember: It is important to have balanced muscle release of both your iliacus and psoas muscles. If you release one and not the other, then they will play tug of war and keep pulling each other out of alignment.
One of the best ways to avoid hip pain while driving is to get to the root cause of your pain. Chances are, if you have hip pain while driving, you likely have hip pain during other life activities as well.
My book, Tight Hip Twisted Core, is an in-depth look at how your iliopsoas muscles impact your daily life. Not only do I provide the background knowledge you need to understand what’s happening anatomically, but I give you the tools you need to prevent hip pain while driving from becoming a recurring issue in your life.

FAQs on hip pain when driving
Can driving cause hip bursitis?
When any muscle is chronically tight, it’s endlessly pulling on both of its endpoints. Both the iliacus and psoas attach to the front of the hip near the groin area. These points where they attach to the bone can develop into tendonitis or bursitis from that muscle being constantly tight. So the tight muscles may be the cause, and driving puts those muscles in a contracted position for an extended time.
How do I stop my hips from hurting when I drive?
While posture and positioning matter, to prevent hip pain when driving you’ll want to learn to release those muscles causing pain during the moments you’re not behind the wheel. Your hip flexors are likely tight and pulling on your hip joints while you’re driving. Understanding how these muscles are affecting your hips, low back, and knees and applying direct pressure to release them will result in pain-free road trips.

Why Do I Have Lower Back and Hip Pain After Surgery?
Remember the song “Dem Bones” from when we were kids? It goes something like, “the backbone’s connected to the hip bone, the hip bone’s connected to the thigh bone, the thigh bone’s connected to the knee bone, the knee bone’s connected to the shin bone…”
While we may associate this song with primary school, there is actually some truth to it (even with the questionable bone-naming).
From our spine all the way down to our ankles, our bones and muscles work together to propel our movements each day. That’s why, if we are experiencing knee pain, it could be associated with an ankle injury or even a tight hip flexor muscle: They’re all interconnected.
When we think about how our body works, especially our lower extremities, we often overlook how interconnected our feet, ankles, knees, hips, and lower back are. But, if your ankle is damaged, it almost always leads to knee and hip pain down the line.
Having ongoing lower back and hip pain can be a symptom or cause of other complications, and can even lead to additional surgeries if left untreated. Understanding how joints and muscles interact as a unit can help you manage your pain following lower back, knee, or foot surgery.
Why do I have pain after surgery?
Surgery is seen as a threat to the body, no matter what kind of surgery. Undergoing surgery takes a significant toll on your overall health, and your muscle-joint interactions as well.
Threats like surgery or injury often cause your muscles to tighten, as an instinctive protective mechanism. During your recovery, your body is likely more stationary than usual as you heal. Your normal walking movements will be altered or assisted, and your muscles won’t engage as readily or in the same fashion as usual, especially if you are experiencing pain. Add-in sleep challenges and increased pain, and it’s natural for your body to want to tighten the iliopsoas muscle and protect the pelvis.
You may have heard of the iliopsoas muscles under a different name: your hip flexors. The iliopsoas muscle is made up of two muscles, the iliacus and the psoas, which work together to perform important movements like walking, sitting, and standing.
The iliacus crosses over your hip joint and attaches to the pelvis, whereas the psoas crosses both the hip joint and pelvis to the spine. If these muscles tighten, they can pull the region off balance by creating a tilt or twist, which can affect your whole lower body and cause lower back and hip pain.
With all the stress your body is going through after surgery, your iliopsoas muscles may tighten to try to support and protect the injured area. Unfortunately, the lower back and hip pain that often accompanies this protective act can be confusing and frustrating when it adds extra pain to your recovery.
But if you had a knee or foot surgery…why are you experiencing lower back and hip pain instead of knee or foot pain? Let’s take a look at how it all connects.
The connection between the lower back and hip pain
Your body is an intricately connected, well-oiled machine. When one piece stops working properly, it affects just about everything. You need your bones for support, your joints to connect them, and all your muscles, tendons, and ligaments to move in the wonderful ways you do.
When one part of the body is injured, weak, loose, or too tight, it impacts how the rest of your body works. That’s why even when you have knee surgery, it can create lower back and hip pain.
The lower back and your hip pain are especially interconnected because of the iliopsoas muscle and the piriformis muscle. If one is too tight, it will add tension to the other, and if one part of your low back or hip is weak, both muscle groups will overcompensate and tighten to protect it.
Since the psoas connects to the spine and works hard to stabilize the back, and the iliacus connects to the pelvis to help stabilize the hip and sacroiliac joint, they’re a primary foundation for both your back and hips.
After surgery, especially hip or knee surgery, your iliopsoas is at a very high risk of tightening and causing an anterior pull. That tug on your pelvic bone strains the connection between your pelvis and tailbone, particularly where the two bones meet.
That junction is known as the sacroiliac or SI joint, and when added tension is put in that area, it gets twisted and irritated, causing lower back and hip pain. If you’re not feeling pain in the SI joint area, then the next most commonly affected joint junction is the hip joint.
The hip socket (acetabulum) cradles your femur (thigh bone) to allow a perfect fit and comfortable movements. When an anterior rotation begins with your pelvis, the thigh bone no longer sits well into the hip socket, and can cause friction or even pull the hip joint out of place.
With or without anterior or internal pelvic rotation, your psoas could also be tightening along with your iliacus. Since the psoas muscle attaches to the front of the thigh bone and the spine at the lower back, it has a similar chain reaction effect as the iliacus muscle as it tightens.
If you have a tight psoas, you are likely to feel a reaction down the leg and up to the spine, but the majority of the tension and pain will be on the spine itself.
A tight psoas muscle pulls your spine into an arched position. This compresses and bends the spine to the side that is being pulled by the psoas. All of the tension and tugging of that part of your spine can easily cause lower back and hip pain.
Leg pain after lower body surgery
Just as with the lower back and hip pain connection, pain from hip to knee is a common issue. An unhealthy iliopsoas, and more specifically an unhealthy iliacus, has a profound effect on pain from hip to knee – as well as the rest of the body overall.
Because a tight iliacus muscle twists the hip and thigh bone, it anatomically changes how your leg connects to your upper body. When the tension in your iliacus muscle is released, your leg and hip alignment will work as designed, but you are far more susceptible to pain when it is tight.
Although the direct connection between pain from hip to knee appears to be with a tight iliacus, that doesn’t mean that the psoas muscle should be ignored completely. After all, together, they form the iliopsoas, so if one is tight, the other is directly affected.
When strain is put on your iliopsoas, it can create a pelvic rotation as the muscle pulls and tightens. This can be either an anterior or internal rotation. Your pelvis’s internal rotation is what could potentially connect hip to knee pain and knee to foot pain.
You can also experience an internal rotation that puts a strain on your knee. An internal rotation of your pelvis affects the way your leg works from the hip down and doesn’t allow the kneecap to track correctly. This internal rotation can also cause the foot to flatten (or pronate), which changes how your foot and toes are aligned.
As you can see, when one area of your body is affected, it can cause a chain reaction of negative effects throughout your body. And, in the case of your lower body, the culprit for lower back and hip pain and imbalance is often an overactive iliopsoas.
So now that we have found the likely culprit for your lower back and hip pain, or your pain from hip to knee, what is there to do about it?
Addressing lower back and hip pain from tight hip flexors
Because of the likelihood of a chain reaction of lower back and hip pain from tight iliopsoas muscles, it is important to address and release them. There are multiple ways you can do this, including gentle strengthening exercises and stretches, and targeted physical therapy.
Strength training for lower back and hip pain
A big part of targeted physical therapy is balancing and strengthening your muscles to recover from – or prevent – future injury. Something you must remember when you exercise in any capacity is that you need equal strength in all of your muscles.
For instance, if you only exercise your front abdominal muscles and neglect your back core muscles, you are far more likely to injure your back or start to develop back pain from a consistent pull from the front of your abdomen.
The same is true for your legs and hips. Finding ways to work all of your muscles to build strength equally can help your body maintain alignment and balance and prevent lower back and hip pain.
Stretching
Stretching and yoga can be a wonderful way to relieve stress, but it can also help as you recover from surgery. After any type of surgery, you will be slightly more stationary than usual, and that can cause your muscles to tense and tighten more than normal.
When it comes to your iliopsoas muscles in particular, stretching can be beneficial. However, you can have too much of a good thing, and if you stretch too much or too deeply, it can cause more harm than good to your iliopsoas.
If you are stretching too much, your muscles will lengthen during the stretching period. Then, once you’re finished stretching, your muscles will begin to tighten again. Additionally, too much stretching can make your muscles too loose, and your muscles will not fully support your joints.
You may wish to consult a physical therapist or other medical practitioner to help decide which stretches will be most beneficial to your lower back and hip pain.
Muscle relaxation for lower back and hip pain
Taking time to relax is imperative to muscle health. Many of us often only find time to relax at night as we are falling asleep, but if our muscles are engaged throughout the entire day and only have one instance of relaxation, it’s not going to be enough to prevent tension from building.
One of the best ways to relax your iliopsoas is to elevate your legs on a couch or ottoman while laying on the floor. This is a traditional restorative yoga practice and can be done for 15-20 minutes at a time.
Consult your doctor about this exercise if you’ve just had hip surgery, as (depending on the entry angle for your surgery) having your hip at a 90-degree angle is not advised for about 6 months.
Another very accessible way to achieve muscle relaxation is to get a professional therapeutic massage. Deep tissue massages can be great for relieving muscle tightness, but they tend to be more invasive and too intense immediately post-surgery. Opt for a soothing Swedish instead!
Muscle release for lower back and hip pain
Releasing muscle tension can help you resolve your lower back and hip pain, and if you are aware of it before you go into surgery, you could even prevent it altogether.
If you visit a physical therapist, they will likely be aware of the complications associated with a tight iliopsoas muscle. A physical therapist can release some muscle tension during physical therapy appointments by putting pressure on specific muscle connection areas with their hands.
However, that is only helpful if you can attend appointments on a regular basis.
Because I don’t want you to have to wait for a physical therapist to help you every single time, I invented the Hip Hook and Hip Release Ball. These tools allow you to release the iliacus and psoas muscle tension you’re experiencing any time you need from the comfort of home.
The Hip Hook’s unique design gives you the ability to apply precise and angular pressure on the hard-to-reach iliacus muscle. The Hip Flexor Release Ball is the perfect size and density to target and help release the psoas muscle.
You can even learn more about realigning your body and treating unresolved pain in my book, Tight Hip Twisted Core.
As you expand your knowledge of how interconnected your joints and muscles truly are, you can easily prevent and treat lower back and hip pain – as well as unresolved pain throughout your body.
FAQs about lower back and hip pain after surgery:
Why do I have lower back or hip pain after surgery?
Along with periods of immobility following surgery, and changes in movement, your body is protecting itself from the trauma of surgery by tightening your core muscles.
But I had hip surgery; why does my knee hurt?
Your core muscles affect the alignment of your entire lower body. If the psoas and iliacus muscles are tight, they will tug on the entire interconnected line from your back, through your legs, and down to your toes. But you can often trace the source back to tension in those core muscles, even though you’re feeling it in your toe.
Why do my hip flexors hurt?
Your iliopsoas muscles may have tightened to try to support and protect the injured area. They work in opposition to the piriformis muscle (deep in your glutes), and when one muscle is tight they begin tugging on each other.
Dr. Bri Talks Lady Bits Podcast – The Effect of the Iliacus on Digestion and Pelvic Health with Christine Koth
Christine was recently featured as a guest on the Dr. Bri Talks Lady Bits podcast, discussing the effect that the iliacus muscle has on digestion and pelvic health. See below for the show notes, YouTube video, and a full transcript of the podcast.
Show Notes:
In this interview with Christine Koth, MPT, you’ll learn all about the iliopsoas muscle group, and in particular, the iliacus muscle… A small muscle that has a BIG IMPACT on digestion and pelvic health. Christine Koth is the author of “Tight Hi, Twisted Core.” Discover how to identify and release the iliacus for less pain and better health!
Watch on YouTube.
Full Transcript:
Brianne Grogan 0:00
I have Christine Koth with me and she has a book that I have with me right here. I know this is going to be on my podcast, if I share it on YouTube, they will see the book. I’m holding it up. But it’s called “Tight Hip, Twisted Core – The Key To Unresolved Pain.” And I got turned on to this book a couple of months ago, I guess. And when it arrived, I literally devoured it, not only because I am an anatomy nerd — I love anatomy — as a physical therapist, of course, I am fascinated by it. But Christine has written the book in such a fun way that it’s really just easy to digest and fun for anybody to read and understand. There’s fun illustrations. It’s a great guide. So the focus of the book is on the iliacus, one of the hip flexor muscles. We’re going to be talking about that today in relation specifically to the iliacus and digestion and pelvic health. So Christine, do you want to say hi, and maybe briefly share why you became so fascinated with the iliacus? And the Iliopsoas muscle group?
Christine Koth 1:08
Yes, absolutely. I’m also a physical therapist. I’ve been practicing for over 20 years and in my practice, I kept seeing this pattern evolve where, you know, as I’m looking at examining people’s bodies, I was noticing that there was tension in this muscle called the iliacus. And that everyone who came into my practice hadn’t really had that addressed. They didn’t even know they had an iliacus muscle. And what I started noticing was that this pattern of tension in this muscle contributing to various conditions. So, today we’re going to be focusing a lot on the pelvic floor, but people were coming in with maybe hip arthritis pain, and they were having tension in their iliacus. Maybe they were coming in with SI joint pain or low back pain, or pelvic floor pain and dysfunction. And then what I was noticing was that this tension was also impacting the mechanics of their body. So, you know, it could be a runner who was having knee pain, and they were focusing on treating their knee, but really, it was coming up from their pelvis and tension in this muscle. So when I started discovering this and started treating it, I kind of developed my own technique of treating the iliacus muscle by putting prolonged pressure on it to try to get it to relax and doing some various physical therapy techniques. And I noticed that oftentimes, for people, this was a missing link. Maybe they had seen 20 or 30 different practitioners, but hadn’t really gotten the relief that they were hoping for. And that once the iliacus was released, it was like the missing piece that wasn’t addressed previously. It was waiting to be addressed and once it was addressed, it really helped them move forward on their healing trajectory. So over time as I continued to realize that this was an area of the body that people weren’t addressing, I kind of took it upon myself to say, “Okay, I guess this is my thing. This is part of what I’m here on this planet to do — is to share information with people about iliacus.” And hence, the development of the book.
Brianne Grogan 3:27
Yeah, and the Hip Hook, which I want to talk about that too. It’s a device specifically designed by Christine to release this muscle yourself. And, I’ve been doing it with my fingers, but I’m really excited to get my Hip Hook because I know it’s going to be a lot easier to release with the tool. And I want to just briefly say that even as a physical therapist who studied anatomy fully — I mean, I know my anatomy, but I will say the iliopsoas is a very challenging muscle group to understand because of the way it hooks into the body. It crosses over so many joints and the way it starts in the back (for the psoas major) and then it goes over the front of the pelvis. Your book really helped outline all of that. Maybe you could give kind of a brief anatomy of where this muscle even is in the body?
Christine Koth 4:22
Yeah, sure. And I’ll share for the video folks a little. This the model as I explain it. It is an interesting muscle because it does cross so many different joints and it goes in a three dimensional way through the body. It’s not very linear. It does attach to the spine. As you can see this is the psoas. The psoas attaches to the spine. It goes through your abdomen — from the spine all the way through your abdomen to the front of your hip and attaches to the front of your leg bone (or your femur). And similarly, the iliacus attaches to the inside surface of your pelvis bone. So, when you put your hands on the front of your hips and you feel that bony part that sticks out, right at the front of your hip — right inside of that is where the iliacus lives. And I have a ton of pictures and stuff up on my website and Instagram and everything, so you guys can examine this yourself.
Brianne Grogan 5:15
And just so everyone knows, if you’re listening to the podcast, I will put links in the show notes to Christine’s pertinent information — website, the Hip Hook, that kind of thing.
Christine Koth 5:26
Awesome. Yeah, so this muscle crosses the spine, the SI joint, the hip joint. And so, it works in a three dimensional way. So it is something that is a little bit mysterious. And the other thing that I will mention too is a lot of people oftentimes group the iliacus and psoas together as if they’re one muscle. They’re actually two separate muscles. They’re innervated by two different nerves. And I think that’s part of the reason why the iliacus might not be addressed as much because people feel like “Well, I’m addressing the psoas so I’m probably also addressing…it’s all the same. And it’s actually not. They’re in two different locations, as you can see. And, they do behave differently and have different effects on the body.
Brianne Grogan 6:13
Oh, my gosh, I have so many questions. But let’s go ahead and dive in. With the connection between these muscles. Well, let’s focus on the iliacus since that’s really what we’re talking about today. But the iliacus on the pelvic floor, because I’ve heard you talk about this before. I read about it in your book. But a lot of the women who listen to my podcast and watch my YouTube have conditions such as prolapse, bladder leakage, and/or issues with pelvic pain and tension. So I know that iliacus concerns can affect all of those issues. But maybe you could tell us a little bit more about the connection between the iliacus and pelvic health?
Christine Koth 6:50
Yes, absolutely. So there’s a couple of different layers to that, if you look at the anatomy, the iliacus is on the inside surface of the pelvis. And in terms of its connection to other muscles, and the fascial connection, it absolutely just connects with the pelvic floor, right? I mean, it’s on the inside of the pelvis and then continues on with the pelvic floor muscles at the bottom of the pelvis and works its way up the other side with the other iliacus.
Brianne Grogan 7:18
So if anyone is listening right now to the podcast and can’t see Christine’s hand, she just described it so beautifully because she’s showing a full bowl effect. Like the wings of the pelvis — the inside of those wings have the iliacus muscle, so those are like the sides of the bowl. And then the base of the bowl is the pelvic floor. So you’re saying that because of the fascial connections, it’s really all connected like this big beautiful bowl, correct?
Christine Koth 7:43
Yep, exactly. If you have any muscle in that bowl that is holding tension, it’s going to affect all the other muscles that are around it. Now the iliacus in particular tends to get tight very easily because its job is to help stabilize your pelvis. So it’s helping stabilize your tailbone to your pelvic bones, as well as helping really to stabilize your hip joint. So I talk about this in the book, there’s many reasons why there could be tension that can develop. It could be from sitting too long. It could be from driving a lot, commuting. It can be from stress — there’s a lot of times we hold stress in our pelvic floor. It’s very common, I’m sure you talked about that. It can also be from certain sports and activities. Like for example, running is very common. Cycling, kicking sports and the like. Also, when you’re hyper mobile. For a lot of women, there’s a good population of us that are hypermobile or overly flexible. And when you have that type of body when you born that way, this muscle tends to kind of hold on for dear life to stabilize you.
Brianne Grogan 8:52
See, that’s a big question that a lot of people have had. So if you have anything else to say about hypermobility, I know people will be interested in that too. Like, well, you know, how come I have these issues when I’m already super loose? Like I don’t need to stretch anything. I know I’m super stretchy so how could I have a hip flexor issue? Or, hip flexor or iliacus tension? So let’s keep talking about the pelvic floor, but if that comes up at all for you, please elaborate.
Christine Koth 9:19
Yeah, we should definitely talk about that. You know what, let’s just talk about that now so we don’t forget because I think it’s very, very important. And then we’ll go back to how the iliacus impacts the pelvic floor. So when people use the word tight, right, and that that word means a lot of different things to a lot of people. I also talk about this in my book — it’s one of my pet peeves. “Tight” can mean one of two things. It can mean either that you can’t lengthen the muscle very well. For example, if you can’t touch your toes means your hamstring isn’t fully lengthening. That is one version of “tight,” meaning the muscle won’t fully lengthen, to allow your joints to move. So when you do a stretch, for example, you are using your own joints to help kind of teach that muscle how to elongate or become longer. There’s another version of “tight” which is holding tension. So you know, this would be an example of like, in your shoulder, your upper trapezius muscle on top of your shoulder — if you touch that, and it’s hard, and it’s not relaxed, that is another thing that people describe as tight, right? So it’s when your muscle is holding tension. Now you can have a muscle that’s holding tension that will completely elongate. But then when you go back to rest, it is still holding tension. And I use the example of, like, if you’re lying down on the ground, and you’re not doing anything, you know, you’re just lying there — you have nothing to do nowhere to go. Theoretically, every muscle in your body should be relaxed. So if you were to touch every muscle in your body, it should be nice and squishy and soft. If you put your hand on the inside of your pelvic bone, and you touch it, it should be just like butter. And if it’s not, then you’re holding tension. So you can be actually very, very flexible. You could go into the deepest yoga pose and not feel a thing but your body could be holding tension in that muscle you could consider as being tight. And the reason that’s important is because if you’re holding tension, and you’re going about your day, that is going to be not only changing the mechanics of your body, you know, muscles should be contracting and relaxing, not just holding tension constantly. And it’s also affecting all the muscles around that. So it is important to discern when you are very flexible, and you can stretch and you feel like “I don’t need to stretch because I’m already really mobile,” you may actually be holding more tension than you think in muscles. It’s a different phenomenon. And that’s where the prolonged pressure comes into play. A lot of times when your muscles are holding tension, you can stretch them and that does help to some degree. It helps increase circulation and helps to get the muscle to be a little bit more healthy. However, it doesn’t necessarily do enough to actually release that tension. And that’s where we use tools like the Hip Hook and balls and rollers and things like that to help your body, learn — your brain basically — learn how to release that tension. So that’s an important distinction.
Brianne Grogan 12:36
You’re talking about that tension and that difference between flexibility and then just the holding tension. It reminds me so much of the pelvic floor and how many people just hold chronic tension in the pelvic floor muscles themselves. And so is that one relation right there, potentially, to the tension that’s chronically held in the iliacus?
Christine Koth 12:58
Yes, absolutely. Like I was mentioning, in this area of the body we hold a lot of our essential organs and a lot of our survival, you know, our procreation is in the pelvic floor. So it’s a very common space for the brain to choose to hold tension in because it’s a protective mechanism. And another common place is at the base of the skull. Protecting our brain, also very important.
Brianne Grogan 13:27
And the reproductive organs, it makes sense.
Christine Koth 13:35
Yeah. So, we don’t even realize that we’re holding tension in that area of the body. You can be sitting at your desk holding tension in that it’s oftentimes related to stress, or even trauma in that area. And we’ve all experienced that on the emotional or physical levels. So that definitely is a big component to that. And the iliacus fits right into that group and that tightness party. Tension party.
Brianne Grogan 14:05
For sure. And so what about prolapse specifically? Do you have any information on that and with relation to the iliacus?
Christine Koth 14:14
Yeah. In a general sense, like we were talking about how, you know, there’s tension in the iliacus, there can be tension in the pelvic floor, or vice versa. It’s like the chicken or the egg? When there’s tension in the muscle, not only does that area not function mechanically, but it also does not function well neurologically. There’s all kinds of nerves in that area of our body that are going to different organs or that are going to muscles. There are nerves that can produce pain, like the pudendal nerve for example. And when nerves are tugged on, or compressed, they are not happy. Nerves do not like to be pulled on and do not like to be pushed on. So in that scenario and that phenomenon, if you have tension in a particular area of the pelvic floor, it can absolutely pull on a nerve and even in just a subtle way. And that tension can make it so that that particular part of your body is not functioning well. For example, if part of the job of your muscles are to hold your organs in place, and you have a nerve or you have muscle tension that is kind of pulling them out of whack, that can definitely impact the function of that particular part of the body. Another thing that’s important too, is that when muscles are tight, they actually become weak, which seems kind of counterintuitive. You think if they’re tight, they’ll be strong, you know, they’re holding tension. But if you’re holding tension for a very long period of time, you can imagine how that muscle would be exhausted. Muscles are the healthiest and most able to produce the force that are required of them, when they can relax and contract and also when they’re in the right length. They’re not being tugged on or pulled out of alignment. So you can see how this is like a complex ecosystem, right? And our pelvic area and pelvic floor — there’s just so much going on in there and really one thing can affect another. You end up with this set of symptoms that you don’t even know how this even started. That’s all it was — I was doing a lot of running and then all of a sudden, my pelvis started hurting, and then all of a sudden I am having incontinence and then the trajectory just goes on and on.
Brianne Grogan 16:27
Well, absolutely. And I want to just briefly share quickly a little bit about my story. I have right sided tension, which is very common. I know that from your book that that’s the most common, correct? And I am right handed and, of course, I drive with my right foot on the brake and the gas, etc. Looking at this condition, now, connecting the dots backward, I was always a runner in college, and in high school. And especially in college, after a few years of driving under my belt, long trips back and forth from college to where my parents lived and that kind of thing. I noticed that I started getting terrible shin splints when I was running. And it turns out, I was horribly over pronating on my right side. So my right arch was collapsing inward for anyone who doesn’t know what that is. And that contributed to shin splints. And so when I got arch supports and better footwear, it definitely helped. But connecting the dots back with my very, very, rotated pelvis on my right side, because of my tight hip muscles, my tight iliacus. That was causing this chain reaction down the road of my leg to actually contribute to that overpronation of that right foot when I was running, and step after step, causing those shin splints. And in addition, tying into digestion, I learned from you this fascinating thing. And who knows, I think it’s connected, that my right sided tension is definitely there. And I’m working on it now. But I have a long standing history of gut issues and one of them is SIBO. And when you said at some point that, because of the placement of the iliacus and the placement of the ileocecal valve, can you go into digestion a bit and the iliacus and particularly SIBO — small intestinal bacterial overgrowth?
Christine Koth 18:27
Yes, absolutely. This is a discovery that I happened to have the opportunity to work side by side a wonderful group of naturopathic doctors in my career. And as you may know, one of the things that people tend to go to naturopathic doctors for is digestive issues.
Brianne Grogan 18:47
Oh yes. I’ve spent many dollars and many, many hours in naturopathic doctors’ offices.
Christine Koth 18:53
Yeah, exactly. So, I started just discovering this correlation. And often the great thing is that these doctors that we’re working with, were super smart. And they were also like, “I wonder if the iliacus is impacting what’s going on here” digestively. So I was seeing people that were having issues with their ileocecal valve not closing properly. And also various digestive issues that can be result of that, but also just other things that are going on. And there is this really interesting correlation. So, again — it’s chicken or the egg — if you have a lot of inflammation in your digestive system, or things are not functioning well, your body’s tendency is going to want to kind of protect that area, right? And so that’s one reason why you could develop tension there. Say you just ate some bad food at a restaurant and your digestion is off for like a day. Your muscles can choose to protect that area because you’re in pain and you’re not feeling well, or something like that, and then that tension can decide to stay there. So then it creates this long term effect where it’s pulling on the nerves and the digestive system is pulled out of whack and all of that. On the flip side, if you have developed muscle tension, which might be like in your situation, you’re talking about being a runner. You know, you develop tension in this area of your body. That tension was pulling on the digestive system itself because of its connection to the fascia because again, the nervous systems connection, and that could have set you up for maybe like a subtle like — maybe your ileocecal valve just wasn’t quite closing well. And then over time, a little bit of the bacteria wasn’t quite flowing in the way that it was supposed to. And then over time, here you are 20 years later with these issues that have developed, just as a result of something being non optimal for a very long period of time. So there’s this definite connection. And what we were seeing in the clinic was that when I would release the tension and the iliacus with my hands, that those patients who are also doing things with their diet, and this supplementation and other things, were actually making much better progress. And symptomatically, whether it was like they were having pain, or they were having issues with their bowel movements, they would notice a direct connection with changes and improvement in that. On those days, when they would work on their iliacus, they’d come back to my office and be like, “Oh my gosh! I actually had a bowel movement and I haven’t had one in like a week.” as a result of that tension. So I think there’s a lot more to explore with that, but there’s a definite there’s a definite connection there.
Brianne Grogan 21:48
I couldn’t agree more. I’m completely obsessed with digestive health. And this has been a long standing issue for me. I think I had it from both ends. I think that musculoskeletally, things were aggravated because of my running and the driving and stress and college and blah, blah, blah, all of that kind of thing. But then I also had a long standing digestive health history as well. So I think it was the perfect storm to kind of, you know, come right in on my right pelvis, really, and make all this happen. But I will say that when I do my release work on my iliacus, just again, using my fingers and I can’t wait for more with the Hip Hook. My gut will start just kind of rumbling back to life in a great way when I work on my iliacus. It’s amazing! Just subjectively, you can add that to your list — things come to life. And I tend to be more slow transit, so it’s really nice to have things kind of come to life when I’m working on that muscle. I did want to ask another kind of personal question also seconded by someone in a group that I lead, which is called FEM squad — one of my FEM squad ladies — she and I both are wondering, can you overdo releasing the iliacus? Can you become a little too aggressive, perhaps? Can you maybe do too much releasing? She kind of maybe went with a little too much gusto and she was feeling quite a bit of soreness. So give us your advice on that.
Christine Koth 23:18
Yeah, so I mentioned earlier how this muscle is a muscle that is not often addressed. Yeah. So whatever age you are — say you’re in your 40s and you’re like, “Okay, I’m gonna start releasing my iliacus.” And you go in there with your fingers, or the Hip Hook or a practitioner and you start putting pressure on that muscle that hasn’t been touched your entire life, do you think it’s going to be happy with you? It’s not, and that’s okay. So it is very common, especially either if you haven’t released it for a long time, or it’s new or you’re new to that — to feel it be very sore. It may feel bruised, like on the surface after you do it and the next day, you may feel sore. You should absolutely take your time and listen to your body and ease into it. There will be a point, believe it or not, where you work on this muscle and you lie on the Hip Hook and you feel nothing. I have experienced that myself. A lot of my clients and people that are using the Hip Hook now experienced that same thing when they first start using it. It’s like “Oh wow, this is really tight and sore and I feel sore afterwards.” That’s great. You know, give yourself time. Give yourself a day or two until you feel like that soreness has dissipated and then you go back to that. You should always listen to your body. If you feel anything that seems completely abnormal or that’s extreme, you should absolutely contact your health care professional and make sure that it’s not something more serious. But it is very common to have that experience. I actually just recorded a video that’ll be up on YouTube, kind of showing people how to use the Hip Hook in a more gentle way to ease into it because when you first start, like I said, it’s very common for that to be very sore.
Brianne Grogan 25:16
I love it. Yeah. And I mean, I think we just get so excited.
Christine Koth 25:23
More isn’t always better though.
Brianne Grogan 25:25
Yeah, yeah, less is more, you can always add more. Okay, well, that’s great. Well, I don’t want to keep you too much longer, because I could just talk to you forever about this. But I do want to ask you, first of all, we know that the Hip Hook is an amazing tool to help release it. If somebody doesn’t have access to that yet — maybe they’re waiting for it, or they aren’t able to get it right now — is there another simple quick tool or technique that you can give them?
Christine Koth 25:52
Yeah, so I talk about it in the book. If you’re going to get at — if you want to address the iliacus itself, different from the psoas. If you want to address iliacus yourself, there’s really only two methods. One is to have a practitioner, or friend, or spouse, or someone put pressure on it. And the reason why this is hard to do, but you can kind of do it your own, like you said, you were using your fingers…
Brianne Grogan 26:16
I use my fingers, or I use my thumb from my other arm, or my other side, and kind of scoop into the area.
Christine Koth 26:24
Yeah. So it’s hard to do that. It’s possible. Your arm will get really tired really fast. And it’s also an awkward angle, not super great for your thumbs and your wrist because you can’t really generate the right amount of pressure at the right angle. And this is my problem. This is why I developed the Hip Hook because I was trying to give people something that they can do at home. You know, when they come into the office — great, I gave them a great release. Fantastic, well, what are they going to do when they get home? And what are they going to do when they don’t have access to me? So I’ve been, you know, playing around with all kinds of tools, like remote controls, spatulas, digging everything you can into that area of the body. And really what I found out was, it just really wasn’t effective as having a person do it, which is why I ended up developing the Hip Hook to try to replicate my fingers so that you can actually do it on your own. But having someone, like I said, a friend or a spouse, push on that muscle across the body, with their arms straight will help to get the right amount of pressure in the right angle, because — I’m showing this on the video, but I’ll kind of try to explain it — the iliacus really lives on the inside surface of the pelvis. So if you lie on something directly, and you push down into the body straight, like, say, if you lie on a ball — actually, that’s one of the things I recommend is using a four inch ball — the ball will get at the psoas and it will get indirectly at the iliacus. But it’s not going to be putting the direct pressure on the iliacus. You really need that kind of angular 45 degree angle, downward pressure to get on that inside surface of the pelvic bone. So yeah, the Hip Hook is really designed to be able to lie on top of it. And then here’s your pelvic bone. Your pelvic bone is on the side. Then with the pivoting of the Hip Hook, it really helps to push pressure directly on the iliacus and get that trigger point release that we were talking about earlier.
Brianne Grogan 28:29
And for the trigger point release, we want to hold for 60 to 90 seconds while breathing?
Christine Koth 28:34
Yeah, and the reason that’s important is because at first, when you first press on it, the body says, “Ouch, I’m tight!” like I’ve been holding tension for a long time, I don’t want to let go, right? And then after about 30 seconds, the brain recognizes that it’s actually in a safe situation, and that it can actually relax some of that tension. So then you’ll notice after that period of time, this doesn’t hurt as bad and is starting to soften. And we want that brain to really kind of recognize that now is the time to change its pattern and choose to let that muscle be relaxed. And that’s really why that length of time is important. Doing it really quickly for a short period of time — it’s better than nothing — but it’s not necessarily going to give you the long term effects that you’re desiring.
Brianne Grogan 29:24
Yeah. Wow, excellent information. It’s so good. I love this conversation and I love learning more about this muscle. I think that more people need to know about it. So I’m glad we’re connecting. How can people learn more about your work and get in touch with you?
Christine Koth 29:42
Yes, absolutely. So I’m on all social media — Instagram, Facebook. Aletha Health (@alethahealth) is the tag so that you can find a lot of information and educational content there. And then alethahealth.com is a website which has a lot of blog posts and videos and information. And there’s also some information on YouTube as well under Aletha Health (www.youtube.com/alethahealth).
Brianne Grogan 30:08
Okay, and what’s the meaning of Aletha? I’m curious.
Christine Koth 30:11
Yeah. So it is the parent company for the Hip Hook, and I developed this company, really to help uncover the simple truth to health and wellness. So Aletha is derived from Aletheia, which is the Greek goddess of uncovering or unveiling the truth. So the Hip Hook is just our is our first product. I have about four other products that are in development right now. And then we’re really curating a whole host of educational content to help people distill the complexities of health and wellness down to their simplest form. Because it’s really a maze out there trying to figure out what works and what doesn’t. And what’s really going to get at the source of your problem or not?
Brianne Grogan 31:04
Yeah, wow. Well, your thought process there is right in line with my thinking, so I love that. And I’m excited to keep in touch. Everyone who is watching, please keep in touch with Christine. Check out her book. I’ll put all of the links in the show notes or video notes wherever you’re consuming this content. And so Christine, thank you so, so much. Is there a final tip or word or anything you’d like to leave folks with?
Christine Koth 31:30
You know, I’m really excited to get this information to you. I would really encourage you to explore your iliacus because it could be the hidden source of what is going on with your body. Wouldn’t it be amazing if it was just that simple? Don’t leave this stone unturned.
Brianne Grogan 31:51
And the root is our source of so many things. And this iliacus is right there with our pelvic floor and the other root components of our body. So, yeah, amazing. Well, thank you again, and we’ll speak to you again soon.
Learn More:
To learn more about the iliacus & psoas muscles and how they may be impacting your body, buy my best-selling book “Tight Hip, Twisted Core.”
Get the Hip Hook:
Get your very own Hip Hook to start releasing built-up tension in your hip flexors, increase range of motion in your hips, and make improvements with your pain.
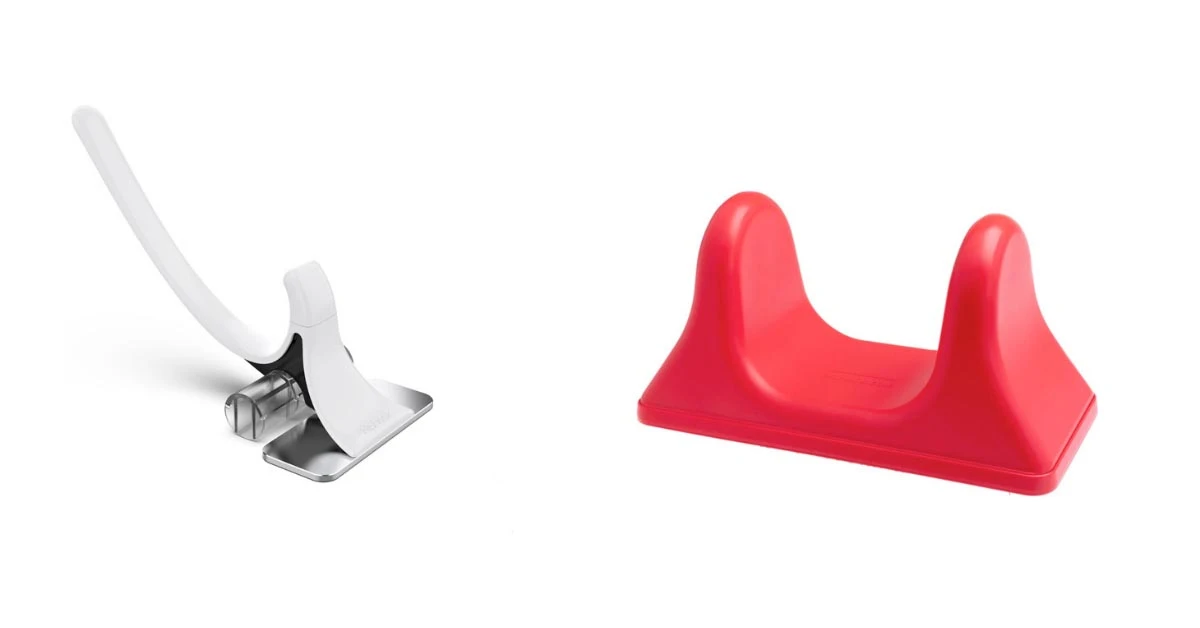
Hip Hook vs. Pso-Rite: Psoas release tool showdown
Here’s what to consider when choosing a psoas release tool.
Do you think your psoas is the cause of your problems or perhaps you know for a fact? In this blog, you will learn about each product’s pros and cons so that you can make the best decision for yourself!
Hip Hook benefits
We will start alphabetically with the Hip Hook.
The Hip Hook was designed by a physical therapist to release tension the iliopsoas (iliacus + psoas). By lying on the Hip Hook, you initially put pressure on the psoas muscle. Once the hook has sunk in and you have relaxed into it, it’s time for the magic. Utilizing angular pressure, pushing down on the lever, results in the Hip Hook pivoting up into the iliacus muscle, effectively releasing both hip flexor muscles.
Think about it this way: if you have tight hip flexors that only tighten up when you stretch them, you require pressure. But you need to apply pressure to both the psoas and the iliacus muscle to release the entire iliopsoas muscle.
Only releasing the psoas and ignoring the iliacus would be like only moving your front tires off the railroad tracks for an oncoming train; you might survive, but it’s not the best decision. There are two parts to the iliopsoas, and the Hip Hook has been designed to use angular pressure and leverage to effectively release both in the same way a physical therapist or massage therapist could do.
For the chart people:

Hip Hook vs Pso-Rite comparison
The Hip Hook is about precision, no different than a sniper rifle. The Pso-Rite is a shotgun. It covers the spread. You can use the Pso-Rite on the glutes, hamstrings, calves, shoulder, pec, biceps etc. This will be perpendicular pressure (straight up and down), and you will not be able to effectively release the psoas and iliacus. Like any problem, you need the correct tool for the job.
Renowned Tri-Athlete Matt Hanson shows us the differences in his ‘Ask the Pro(f)‘ breakdown.
Bobby & David briefly describe the differences between the two products.
Pso-Rite vs Hip Hook review
The makers of the Pso-Rite brought psoas release into the mainstream, and we are so thankful for that. If you purchase the Pso-Rite and it provides you relief, that makes us so happy, as that fits with our mission of ridding the world of unnecessary pain.
The hip flexor complex is, well, complex. What may work for you may not work for others. That is why we genuinely want you to find the best tool for you! The Pso-Rite may work on your psoas, but it can’t reach the iliacus effectively because it wasn’t designed to do so.
If you have general hip or quad tightness and it’s not causing you pain or getting in the way of your life, the Pso-Rite may be a good starting point as it allows for use elsewhere in the body.
Now, if the Pso-Rite didn’t work for you, or if your hip flexors are causing pain in the hip, back, down into the knee or even up into the ribs, shoulder or neck, then you NEED a precision tool to get at the muscle effectively to relieve that long-standing tension.
We only hope to provide the correct information so that you make the most informed decision. Please do not hesitate to contact us with your questions via our Instagram or contact us directly info@alethahealth.com to see if the Hip Hook is right for you!
You can get The Hip Hook alone or bundle all of our products together in the #FixYourHipKit, which comes with the book, Tight Hip Twisted Core (the guide to solving your pain), the Hip Release Ball (a massage ball that can help you release the low back, glutes, and other muscles of the body), as well as the Hip Resistance Band (a loop band to help strengthen your glutes and outer hip muscles).
Happy Hip Healing!
Frequently asked questions about the Hip Hook
How does the Hip Hook work?
The Hip Hook is a psoas release tool and iliacus release tools designed by physical therapist to specifically address muscle tension and tightness in your hip flexors. Using your own body weight to apply pressure to your muscles, you will first lay yourself over the tool with the platform of the Hip Hook flat on the ground to address the psoas. Then, by reaching back with your arm to press down on the handle of the Hip Hook, the tool will rotate and be pressing on the iliacus.
How does the Hip Hook compare to other hip flexor release tools?
The Hip Hook is different because it is designed to release BOTH the iliacus and psoas muscles – the 2 muscles that make up your body’s main hip flexor, the iliopsoas. Other hip flexor release tools or balls primarily address the psoas muscle without giving the proper attention to the iliacus. Releasing both of these muscles may lead to better and longer-lasting results compared to releasing the psoas alone.
How does the Hip Hook compare to a massage therapy ball?
Due to its rounded shape, a massage therapy ball can apply broad pressure to the psoas muscle and may have difficulty accessing the iliacus muscle on the inside surface of the pelvic bone (or ilium). The Hip Hook has a tip that can apply more precise pressure to the psoas muscle and also has the ability to rotate and access the iliacus muscle at an angle.

What is the Current Hip Hook Promo Code?
People are asking for a Hip Hook promo code, so we’re making a special little spot on the internet for you to check out the current deals on the Hip Hook, Hip Release Ball, and the bestselling book: Tight Hip, Twisted Core. You deserve the best deal we can offer, and we fully support an investment in your health.
We’ve replaced a Hip Hook promo code with special package deals just for you.
Here are Aletha’s current Hip Hook promo deals:
The #FixYourHipKit – a bundle of all three products for maximum pain reduction, PLUS the tools to prevent future tension and injuries.
Just want the Hip Hook ? Lucky you: for a limited time, you’ll get a discount off the regular price.
Both deals include free ground shipping in the United States.
Now is a good time to fix your hips
This year has not been kind to our hip flexors: from additional stress to less-than-comfortable work from home situations. Our hips and backs need some much-needed attention. That is why we are offering all of Aletha’s products bundled into the #FixYourHipKit at a discount as a Hip Hook Best Deal.
What’s going on with my tight hip? Why can’t I figure out this lower back pain?
Based on decades of study and clinical practice, Tight Hip, Twisted Core gives you the 3 Simple Steps to live a pain-free life without surgeries, medications, or thousands of dollars. This book explains the major causes and patterns that lead to hip and back pain, along with the exercises and adjustments to relieve tension and prevent future issues. It’s an owner’s manual for your core muscles and a complete guide to using the Hip Hook and Hip Release Ball.
The Hip Release Ball, included in the #FixYourHipKit Hip Hook Deal, is the perfect size and density to provide effective release of the general area around the iliacus and psoas muscles, and the perfect warm-up for the Hip Hook. The ball can also be used to help relieve tight muscles at the back of the hip, glutes, piriformis, hamstrings, and low back muscles. If you are super-tight, the ball is going to allow you to comfortably access all the nooks and crannies of your hip and glute muscles with broad pressure.
Benefits of Rreleasing the psoas and iliacus muscles
The Hip Hook is the world’s first tool designed to specifically release tension in the iliacus muscle and address the root cause of the problem. These are muscles that can only be reached through specific, angled pressure.
- Precise height to allow the perfect amount of pressure
- Tip can pivot to provide pressure to the iliacus where it attaches to the pelvic bone
- Weighted with a gripped bottom for precise placement
- Rubber angled tip to be effective but comfortable
It eliminates tightness at the core of the hip flexor and quickly reduces strain in the legs, hips, and lower back.
The psoas and iliacus have been labeled as the most vital muscles in your body, and these tools can reduce iliacus and psoas injuries for runners and reverse the damage done by prolonged periods of sitting.
Take advantage of the Hip Hook Promo Codes (follow the link to the best Hip Hook deal!) and let’s get you back to running, playing, living, and laughing again.

Why Do I Get Hip Pain From Stretching? For Dancers, Gymnasts, and Yogis
Hypermobility is encouraged in yoga, dance, and gymnastics. But if you’re naturally flexible and are someone that has no problem reaching – or reaching past – your toes, you may be just as susceptible to a hip pain as someone who regularly experiences hip flexor tension and/or lives a sedentary lifestyle.
In fact, you can actually be too flexible. And, yes, your stretching may be causing hip pain.
Let me explain.
You have two large muscles that are central to the movements you do every day. Your psoas muscle and iliacus muscle sit side by side and run from your spine to your pelvis to your thigh. Together, they are called the iliopsoas muscles, and they allow you to sit upright in your chair, drive a car, go for a morning jog, balance on a high beam, do a forward fold, learn a new four-count, and more.
The iliopsoas is in a compressed position when you bend forward, sit down or pull your knees up. And, for many people with tight hips or hip flexor pain, it’s a result of keeping these muscles in that shortened position for too long. It causes your iliopsoas to hold that position – sometimes even after you straighten your legs or stand up.
If you’ve ever felt stiff in your hips after a long day at your desk, this is what’s happening. Parts of your iliopsoas have not effectively relaxed after use, and they continue to pull on your pelvic bone and spine.
This whole idea of opening up the hips and creating more space in the hips is an idea that is useful for people who have a lot of tightness. Some of us tend to be really stiff and tight and need more flexibility, and yoga is a great form of exercise for those kinds of bodies.
In contrast, those who are already really mobile and can easily get into a deep lunge or fold forward with their hands to the ground already have a very flexible hip and do not need their hips opened more.
In fact, hips are designed to be stable and when they become too loose, your muscles tighten up to try to keep you from falling apart. It seems counterintuitive, but in this situation, a tight iliopsoas muscle is the result of your body trying to stabilize itself after overuse or too much mobility.
Let’s take a closer look at what’s happening in your hips as a very flexible person.
What causes hip injuries in yoga, dance, and gymnastics?
People who are naturally inclined to be more flexible may find themselves drawn to sports and activities that let them highlight that strength and continue to strive for a deeper stretch. If you’re a dancer, gymnast, or yogi, you probably have those “goal postures” you are working toward, like the splits, a deep pigeon pose, a flatter forward fold, or kicking your legs up to your nose.
And, when that’s the goal, more flexibility is revered.
However, these extreme motions are well past a normal range of motion for your body. They bring the lower back, hips, and pelvis into positions that are outside of what these joints are really designed to do. And, though they may be accessible to you, repetitive motions, swift movements (such as when dancing), stretching unevenly from side to side (if you favor one side over the other for the deeper postures), and continuing to move into these deep stretches day after day can and do strain your joints and the tissue that holds those joints together.
Even when you take out the swift extension and compression of your muscles, such as in gymnastics or a dance routine, you can still stretch too far. People sustain some of the most common yoga injuries because they are pushing past hip tension. What feels like a sense of accomplishment and that oh-so-sweet depth is setting the stage for problems early on.
This is why most people end up with yoga injuries after about 5 years of practice. Too much mobility has been developed.
With too much mobility, long-standing tension in the iliopsoas muscle develops. It is tightening its grip around your pelvic bone, hip joint, and spine in order to stabilize your core during a stretch or movement.
You see, your iliopsoas muscles are designed to protect your tendons and joints in this region, this is their primary job, so when you’ve created an unstable area to protect, they rise to the occasion.
Your iliacus muscle crosses over the hip joint, attaches directly to the pelvis, and affects the SI joint. The psoas crosses over both the hip joint and the pelvis all the way to the spine. Normally, your iliacus and psoas are responsible for moving these bones – I like to think of them as “puppets.”
But when your muscles become fatigued and are faced with the job of keeping this area from falling apart, they choose to contract and develop knots and tension that stays there not just during your yoga practice, but throughout your life.
This constant tension results in this part of the body taking on more stress and friction than it was designed for.
Furthermore, constant tension in the iliacus and psoas pulls on the pelvic bone and spine, changing the alignment of the hip, SI, and spinal joints and that mechanical change works its way down to the feet and up to the head. Because these muscles are at the core of your body, they affect everything else around them, even creating tension in other muscles in the glutes, hips, and spine that end up playing tug of war with them.
Therefore, that hip flexor pain or tension you feel is really a signal from your iliopsoas that you’ve gone too far. If you push past what your joints are meant to do, you may be inviting a dance, gymnastics, or yoga injury.
Three common hip problems due to hypermobility
There are various injuries or disorders that can cause a dancer, gymnast, or yogi to experience hip pain. I chose to focus on the three most prevalent problems I’ve seen happen in stretching sports.
Hip impingement
Hip impingement, or femoroacetabular impingement (FAI), occurs when the hip joint movement becomes restricted by the abnormal contact between the ball and socket bones.
A hip socket (acetabulum) is usually quite deep, stabilizing the ball of your femur during movement. This ball and socket joint is reinforced and protected by a lining and ring of fibrocartilage.
When there is a change in shape (such as with a bony growth or genetic malformation), a misalignment from the bones being pulled on by the iliopsoas muscles, or excessive use of the hip joint (such as in ballet) it causes unnatural friction. Movements can become extremely painful and piercing, which eventually restricts movement.
Hip dysplasia
To maintain a high intensity of hip mobility during dance, gymnastics, or yoga, many female participants actually have very shallow hip sockets. This could prevent them from ever experiencing hip impingement, but it could cause hip dysplasia instead.
Whereas a deep hip socket adds structural integrity to your movements, a shallow hip socket can create instability and put added stress on your hip flexor muscles. Athletes with hip dysplasia rely very heavily on the labrum (fibrocartilage) and soft tissues around the hip during movements like flexion. Because of this inherent instability in the joint, the muscles around the hip often present with excess tension to compensate.
Most dancers or gymnasts that have hip dysplasia may indeed be very flexible, but they are also more likely to experience a labral tear, hip flexor tendonitis, and cartilage damage as well as the host of issues that come with a chronically tight hip flexor.
Osteoarthritis
We often associate arthritis with old age, but early-onset osteoarthritis has increasingly become an issue among young gymnasts, dancers, and avid yogis. There is evidence to suggest that young, athletic people develop it due to consistent stress and overuse of their hip joints.
For example, a grand plié in dance or a malasana (garland pose) in yoga are both movements that require an extensive range of motion within the hip region. Other movements similar to this can further increase the severity of hip impingement or another hip injury (i.e., labrum tear), leading to osteoarthritis at an early age.
Hip impingement is such a big player in osteoarthritis development because osteoarthritis occurs due to the wear of cartilage tissue in your joints. As cartilage is damaged, and additional friction is applied, osteoarthritis develops and worsens with time.
If you are experiencing early symptoms of these hip injuries – or have already been diagnosed – it’s time to gain more stability before returning to those deep postures and swift movements.
Seeking stability and balance for your iliopsoas muscles
The idea of balance, both mind and body, is well-touted in yoga, dance, and gymnastics. However, we often forget what that looks like in regards to our iliopsoas muscles.
As a very flexible person, the solution may be the opposite of others experiencing hip pain.
The mainstream thought is that, if you are experiencing hip tension, a nice hip opener or yoga for tight hips may help. And hip flexor stretches are very valuable for someone who isn’t experiencing or using their full range of motion yet.
Ironically though, a very flexible person may only experience more hip tightness as they continue stretching.
That’s because those who are already really mobile and can easily get into a deep lunge or fold forward with their hands to the ground do not need their hips opened more. What you need is stability and strength in and around your psoas and iliacus muscles.
Now, you may have just learned what your psoas and iliacus muscles are. However, if you regularly partake in a sport that requires deep stretching and hypermobility, you can seek balance by slowing down, listening to your body, introducing stability exercises and learning how to release your hip flexor muscles.
Four yoga injury prevention tips to help you avoid hip flexor pain and tension from overstretching
The good news is, most hip-related gymnastic, dance, and yoga injuries are preventable, or at the very least manageable.
But it can be challenging to navigate the sensations you are feeling in your hip flexors – and to know whether you need more or less stretching. Here are some general tips and practices to abide by in order to enjoy your next gymnastic competition, dance practice, or yoga flow pain-free.
1. Perfect your technique, form, and feel
Many dancers and gymnasts start at a very young age. This can be both good and bad for technique. If you had a competent teacher during that time, they would have corrected your technique.
However, that is not always the case.
I have seen clients doing a stretch incorrectly for years, even causing damage, because they didn’t clearly know what they were supposed to feel. Many people who begin stretching or want to become more flexible view tension and slight pain as a sign that their efforts are paying off or they are working new muscle groups.
You know, “no pain, no gain.” But when it comes to your hip flexors, that could not be further from the truth.
If you are feeling pain or tension in your postures and movements, it’s time to re-evaluate your form and become aware of any bad habits you’ve picked up. Understanding what kind of sensation you should be feeling with a certain motion and where will help you evaluate if you are feeling something you shouldn’t.
For example, if you are in a deep hip flexor lunge stretch and you feel a stretch in the muscle in the front of your thigh and front of your hip, that’s an appropriate sensation for that motion. In contrast, if you feel a sensation in the back of the hip or your spine, that’s not good. Similarly, a deep, dull pull in your hip joint could indicate that you are stretching your joint capsule and not a muscle. Joint capsules are not supposed to be stretched.
This may mean enlisting the help of a new coach or teacher. And it may also mean backing off deeper stretches and advanced motions until your body can re-learn what the correct feeling is.
Slowing down to identify and correct improper technique or form will be only a temporary setback that wields long term success and may even prevent an injury.
2. Listen to your body
All of us have a different composition of collagen (the connective ‘stiff’ part of your tendons and muscles) and elastin (the ‘stretchy’ counterpart of collagen) in our bodies, as well as a unique ball and socket shape in our hip.
That means that a leap, hip flexor stretch in yoga, or plié will look a little different from person to person.
Chip up, buttercup, that’s perfectly okay and natural!
When you hold a yoga pose or perform a dance routine, your body will sometimes communicate with you. These messages of slight pain or a sudden loss of strength are not to be ignored.
For example, if you are in pigeon pose or performing a deep hip flexor stretch during yoga, and you begin to feel pain, do not just breathe through it and hope for the best. That is your iliopsoas or joint speaking up and telling you that your body is not ready to be stretched that deeply in that moment.
You may simply need to take it easy that day or invest more time in your warm-up routine. But, if ignored, stretching too intensely can easily cause a muscle strain, tear, or increased hypermobility of the hip muscles.
3. Balance your strength training
Ah, that word balance again.
It’s so important to make sure you are stretching and strengthening your muscles in equal and opposite ways. For example, if you favor one leg when going into a cartwheel, make sure you are also strengthening your other leg. And, when you do a forward fold, balance the movement with a sphinx pose or similar movement that stretches the front of your body.
Your psoas and iliacus muscles are quite capable of holding you and propelling you through poses and dance moves. But, that doesn’t mean they should bear the brunt of the force alone. Stronger glutes, thighs, and abdominals will help stabilize your core even more.
Keeping these muscles evenly conditioned with cross-training will help your body spread out the impact of explosive dance moves and deep stretches.
4. Know when massage isn’t enough
Massaging and tending to sore or tight muscles is important for rest and recovery. It can help break up scar tissue from prior injuries, increase muscle circulation, and relax your mind after a difficult workout.
As an athlete, you’re probably no stranger to professional sports massages as well as self-massage techniques such as foam rollers, balls, and other tools that move or vibrate. However, if a tight iliopsoas has already caused a trigger point or muscle knot, massaging that part of your muscle will likely activate and aggravate it further.
This can actually worsen your hip pain from stretching.
If you’ve reached this point, only a full release will help you get the relief you are looking for.
To do this successfully on your own, you will need a tool like the Hip Hook – or a skilled practitioner – to locate the exact spot where your iliacus muscle connects to your pelvic bone. That’s because your hip flexor muscles are considered inner muscles, and can be very difficult to locate with your own hand. Additionally, a full release requires a precise amount of pressure at a particular angle that you can’t achieve by just lying on a particular tool.
The Hip Hook replicates the motion of a skilled physical therapist, using only your body weight and a lever to apply pressure to and encourage a release of the psoas and iliacus muscle.
This tool and technique is crucial to not only the health of the psoas and iliacus, but for happy hips, SI joints, pelvises and lower backs. Keeping the hip flexor muscles relaxed as you continue with these hypermobile activities, can prevent or help heal injuries in these areas as well as issues up or down the kinetic chain, head to toe.
In addition, happy hip flexors, the Hip Hook actually helps with performance enhancement in dancers, yogis, and gymnasts. When these muscles are not holding tension, it allows for the hip flexors and all the muscles around them to be strong and mobile.
So if you are working on a deeper split, releasing your hip flexors with prolonged pressure using the Hip Hook will stop the tug of war with the hamstring, for example, and allow for a deeper split.
If you are a seasoned gymnast, dancer, or yogi, it may take a bit more time to get to the level of release and pain-free movement you want. However, this is a natural remedy to hip pain that you can practice daily before and after your practice to promote a happy, healthy, and flexible iliopsoas muscle.
Take time to learn more about hip injury prevention
Having a hyperflexible hip can feel like both a blessing and curse. But when your hips start to develop a problem, it is not something to take lightly. Listen to what your body is telling you, and take steps to prevent future hip pain from stretching.
Empowering yourself with accurate information about the anatomy of your hip muscles, tendons, bones and joints, learning more about the correlation between stretching and hip pain, and practicing movements that balance the more flexible postures with strengthening can help ensure your dancing, leaping, and downward dog-ing for years to come.
Want to keep learning? I talk about issues all these issues and more – and provide multiple solutions that I’ve seen work after years of being a physical therapist in my book, Tight Hip Twisted Core: The Key to Unresolved Pain. Interested in the Hip Hook? See why professional dancers all over the globe are excited about it!
Frequently asked questions about hip pain and hypermobility
Can hypermobility cause hip pain?
People who are hypermobile or are very flexible have the ability to move their joints beyond a “normal” range of motion. Their surrounding muscles, tendons, and ligaments may exhibit more laxity where it makes the hip joint less stable. This instability can increase the likelihood of pain or injury when moving within those extended ranges of motion.
How can I prevent injuries if I am hypermobile?
To prevent injuries if you are hypermobile, it is important to work within a range of motion that you can actively control. This idea focuses more on strengthening your muscles at your end ranges of motion instead of stretching. Examples of this could be shortening your stance during yoga poses or reducing the depth on your squats, moving slowly and with control to ensure that your muscles are engaged to support you in those positions.
Should I stretch if I am hypermobile?
If you are hypermobile, the muscles and joints in your body are already very flexible. Continuously stretching can lead to over-stretching, which makes your joints less stable. The surrounding muscles may respond by holding tension in an effort to protect the body and create stability. While some stretching can still remain a part of your routine, you may experience more benefits in how your muscles and joints feel by adding in more strengthening and muscle release.

Managing Hip Pain While Cycling
My clients that are cyclists often report persistent – sometimes even debilitating – hip flexor pain before, during, and after cycling. And, while riding a bike may have a lower impact on your lower leg, it can lead to back, hip, and knee pain.
Hip flexor pain with pedal clips while cycling
When you’re cycling and using pedal clips, your hip flexors are staying continually engaged with every revolution of the pedal. While one leg is pushing down, the other is pulling up, all the while asking for posture and stability in the core. This keeps the hip flexors (iliacus and psoas) working very hard in a shortened position. Muscles don’t like to be in a short position, they cannot generate the same amount of force and they tend to shorten and tighten over time.
This is felt the most at the groin where the hip flexors attach to the inner thigh. It can also translate into glute pain, sciatica, pelvic floor pain, back pain, SI (sacroiliac) pain, or knee and foot issues. Cycling is a very similar movement as pulling your knees up to run or holding a boat pose when doing ab workouts, activating the same muscle group in your lower abdomen.
During this entire time, your hip and core muscles are also remaining contracted to hold your position on the bicycle, balancing you from left to right, forward and backward.
So, that’s why your lower abs probably hurt a lot more than you expected when you first started cycling – and why you may be feeling hip flexor pain when cycling now.
So, if you’re a cyclist, what can you do about the pain – and how can you prevent it from turning into a larger injury?

Getting to the root of hip pain from cycling
To manage hip pain from cycling, it helps to understand what causes it in the first place.
Endurance sports like running, swimming, and cycling all have a relatively high risk of injury due to the fact that you are requiring your muscles, ligaments, and joints to be in constant motion during extended periods of time. When you’re biking for miles on end, even if you maintain ideal form, the repetitive motions can put enormous strain on your muscles and joints.
Keeping this in mind, there are usually three main culprits for hip pain caused by cycling: overuse, muscle imbalance, and improper bike fit.
And, as you’ll see below, all three of these often cause the same result: tension and tightness in your iliopsoas muscles, which are a pair of muscles that sit side by side and run from your pelvis to your inner thigh. This overuse in a shortened position causes them to revolt with long-standing tension.
This tension is often the cause of not only hip pain, but pain in this region from cycling.
Tight iliopsoas for cyclists
One of the most common causes of hip pain for cyclists is overuse. Each time you pedal, you are engaging your iliopsoas muscles in opposite directions, either stretching them to extend the pedals or contracting them to pull up on the pedals and propel the bike forward.
While your iliopsoas muscles were made to extend and contract, they were not designed for doing this motion continuously for hours at a time and in a shortened position. Muscles don’t function well when they are too short or too long, they are strongest in their optimal length. In addition, the hip flexors work to stabilize your pelvis and spine in a somewhat stable position while your legs move underneath you, requiring even more from this cramped duo.
Without muscular endurance, your hip muscles will not be able to properly support your hip, back, and pelvic ligaments and joints. And, if you are quickly adding miles day after day with little to no recovery time in between, your fatigued hip muscles may be inviting pain and injury to the surrounding tendons, ligaments, and joints they are supposed to be supporting.
Muscular imbalance in the pelvis and psoas
Any time you are extending and contracting your iliopsoas muscles in opposition – such as when one leg is pushing the pedal forward and the other is pulling up from behind – there is an opportunity for an imbalance to form.
This is very common – and not just with cyclists. Most people have one thigh or glute that is dominant or one hip flexor that is tighter than the other.
You may not even notice yourself using one more than the other when walking or sitting in a chair. But, when you are cycling, you could be unknowingly putting more stress on your dominant leg. Your body may try to correct the imbalance after you get off your bike. However, this often results in one leg feeling excessively tight the next day.
The tightness likely began near the top of your pelvis, where your iliopsoas muscles connect to your hip joints. If they are pulling too tightly on your pelvis bone, it will affect the entire mechanics of your spine, pelvis, and hip. The muscles in your thigh may even feel sore and it may even be pulling on your knee joints, causing knee stiffness, and pain.
Improper bike fit and iliopsoas tension
Even if you have great muscular strength and balance in your legs, glutes, and hips, you may still suffer from hip flexor pain. One of the most common causes of hip pain during cycling – and sometimes the cause of muscular imbalance and overuse – is an improper bicycle fit.
When your bike isn’t professionally fitted to your body, it pushes your posture and body angles into unnatural positions.
Your muscles will try to overcompensate for the abnormal positioning. But, this can lead to one or both iliopsoas muscles being contracted too much or being used unevenly.
For example, think about the position of your pedals.
As a general rule, a 90-degree angle is a good range of motion for your hips and knees. So, if you are too compressed on your bike and bringing your knees up past your hip joint, you are overexerting your iliopsoas muscles, again, asking them to work hard for you in a compromised position.
Conversely, having your seat post too high can cause you to reach too far for the pedals, resulting in excessive motion and strain in the pelvis and spine while riding.
So now you know what causes hip pain while cycling, here are a few tell-tale signs your iliopsoas muscles are being overworked.
Common hip flexor issues for cyclists
The four most common hip flexor issues for cyclists include:
1. Snapping hip syndrome in cyclists
Also known as hip flexor tendinopathy, snapping hip syndrome causes a painful clicking in the hips. This “clicking” will usually be accompanied by a feeling of your tendons pinging. Most often, the click will be both a painful feeling and an audible noise, but it can manifest in just an audible form.
This pain is commonly the result of someone who is not naturally flexible overusing their hip flexors – or someone who is naturally flexible pushing their muscles too far. The snapping sensation and sound can be a result of a taut muscle, usually, the iliacus, psoas, or TFL, clicking over a part of the bone that sticks out nearby. This snap can also happen inside the hip joint itself. When there is hip flexor tension, the alignment of how the ball of the hip fits into the socket is off, making the joint click.
2. Hip bursitis in cyclists
Trochanteric bursitis is a common hip ailment that impacts many athletes, not just cyclists. It is a type of chronic pain that is caused by friction and inflammation of the bursae along the outside of your hips.
Each of your hips has two major bursae, which are small fluid-filled sacs designed to help reduce friction in and around your joints. They are there to protect the tissues from wearing down with motion and rubbing. But, when your muscles are imbalanced or overused during exercise, the bursa areas experience uneven strain and excessive friction, which causes inflammation.
If you notice pain on the outside section of your hip that extends to the upper thigh area, you may have hip bursitis.
The pain may begin as a very sharp, intense pain, but over time it could fade into a dull, wide-spread ache. You may even notice some swelling, warmth, or redness in the hip area.
3. Piriformis syndrome in cyclists
Piriformis syndrome impacts the buttock’s piriformis muscle, a muscle that sits directly opposite your hip flexors and iliopsoas muscles. So, when your hip muscles are pulling your pelvic bone forward, the piriformis muscle may contract in an effort to balance the strain. It’s a mean version of tug-of-war.
This then irritates the sciatic nerve, often causing pain to manifest in your hip area. Sciatic pain can be very insidious, starting as numbness or sharp pain in the buttocks, slowly creeping into your hips, lower legs, and even your feet.
4. Hip impingement syndrome in cyclists
Femoroacetabular impingement is one type of hip impingement syndrome. Impingement pinches the tendons, joint capsule, and labrum in the hip joints, usually due to the unique shape of your ball and socket in the hip. This creates a pinch during movement.
This happens often in cyclists because the hip joint is in the flexed position for extended periods of time – and that’s the exact position that pinches.
Repetitive motions like cycling tighten your iliopsoas muscles, causing the joint to be compressed and out of alignment, pinching the joints. This extra stress and inflammation are often all that’s needed for hip impingement to occur.
Hip impingement is noticeable as it can inhibit your range of motion and cause a distinct pain in the front of your groin. At first, the pain in the hip flexor and groin area may feel dull and achy. But, as it worsens, the pain will occur with more subtle movements and can be sharp as well.
How to improve hip health while cycling
Having a doctor or physical therapist diagnose your hip pain is the first step in working towards hip health, and hopefully, pain-free cycling.
While anti-inflammatory and pain medications can help ease some symptoms early on, becoming dependent on medications will usually only treat the symptoms, not the root cause.
I’m much more inclined to help my clients get to the root of the problem and find long-lasting results. Especially because releasing your iliopsoas muscles and keeping them in a happy state while cycling doesn’t have to be difficult.
7 ways to alleviate your cycling hip pain
Here are some tips for regaining pain-free cycling sessions.
1. Use bike gears properly
Knowing how to ride your bike is one of the most basic yet influential aspects of avoiding hip pain while cycling. If you are misusing your gears, you will exert more effort and put more strain on your hips than necessary.
2. Get a bike that fits
Professionally-fitted bikes drastically improve your posture while riding. Knowing how to fit your bike is difficult, so I recommend getting a professional opinion. They will be able to take photos of you sitting on your bike and can explain what the position for optimal riding comfort, performance, and efficiency feels like.
3. Warm-up before cycling
Your leg and hip muscles have a lot to do with your cycling ability and performance. You are pedaling with them, after all.
Just as with other forms of exercise, a proper warm-up prepares your muscles for the hard work ahead. It gets the blood flow going to your joints and ensures that your muscles won’t be as susceptible to tears or twists.
You want to try low-impact exercises that engage your legs, glutes, and core muscles before you ride. Yoga can be a great warm-up option for cycling, as well as lunges or planks.
4. Stretch often
Just as warming up before a ride is important to get your muscles and joints ready, stretching is an integral part of recovery. After any exercise, stretching highly-used muscle groups helps prevent muscle soreness and tension.
However, it’s very important to not mistake tension for a sign to go deeper into your stretch. Be gentle with your iliopsoas muscles and respect the range of motion that your body has.
And remember, there is no rule that you can only stretch after a bike ride. If you experience hip flexor tightness or pain, stretch as often as you want, whether that be before workouts, during workouts, after workouts, or on your off days.
5. Try the Hip Hook
Stretching is often not enough to change the tension holding patterns that may have developed over time. For a full and lasting iliopsoas release, you really need a tool such as the Hip Hook.
The Hip Hook helps you find the exact location of the psoas and iliacus where they connect to your pelvic bone and let you use the weight of your own body to apply the right amount of pressure at the exact angle needed for a release that only a skilled professional can reproduce.
This is an essential step when it comes to relieving pain and tension in the hip flexor region. Without this tool, it’s nearly impossible to release your own iliopsoas muscles, and you may need to seek out a good manual therapist or practitioner to help you.

6. Use a foam roller
With any muscle soreness, foam rollers come in handy. For large areas like your legs, foam rolling is an excellent way to add the benefits of massage to your cool down or stretching routine.
While a foam roller can’t effectively reach your hip flexors for a full release, you can focus on muscle release above your knees, and on the outside of your leg.
Although it’s tempting to roll out your IT band like everyone else, remember that the IT band is a piece of fascia that should not be rolled. It can’t be “tight,” only the muscles that attach to it can be tight. Instead, focus on the glutes and TFL muscles to fix IT band pain. Tightness in these muscles that attach to the ITB can worsen symptoms of bursitis and cause additional hip pain from cycling.
7. Balance your muscles
An imbalance of muscle strength can be a big issue. Finding time to cross-train and target areas like your hips, legs, and glutes to balance out strength is extremely important.
Exercises like planks, squats, low lunges, bridges, pelvic tilts, and many others are useful. Just be sure that if you are working one muscle area, you exercise the opposing muscle group as well. Additionally, you can get an analysis of how you use your muscles while cycling – often at the same time you are getting fit for your bike. A professional will be able to analyze a heat map of how you are applying pressure in the pedals and whether you tend to favor one leg more than the other.
They can then work with you to help you reach more of a balance.
Find the key to unresolved hip pain
If you are experiencing hip pain while cycling, it doesn’t need to become a chronic issue. There are many ways to remedy hip flexor pain, from balancing your muscles to ensuring proper bike fit. But remember, the key to reducing hip flexor pain while cycling is to listen to your body’s limits.
Good form and balance tend to be compromised when you are tired.
And this is when your iliopsoas muscles, ligaments, tendons, and joints become more vulnerable.
For more precise steps you can take to solve your hip pain when cycling, check out my book, Tight Hip, Twisted Core – the Key to Unresolved Pain.
Frequently asked questions on hip pain while cycling
Is cycling bad for the hip flexors?
When cycling, the hip flexors are placed into a shortened position and are constantly being used throughout the course of a bike ride. This constant and repetitive action through this reduced range of motion may increase the chance of the hip flexors becoming tighter, especially if these muscles don’t adequately recover. Consider adding in some exercises to stretch and release tension in the hip flexors to reduce the likelihood of developing hip pain while cycling.
Why do I get hip pain when cycling?
Cycling places the body into a forward-leaning, seated position for extended periods of time. As you continue to put your body into this position and use the same muscles, there is an increased chance of developing imbalances that ultimately impact the alignment of your body. Over time, this can lead to the surrounding muscles tightening up and creating compression around the hips, and cause pain.
How do I stop my hips from hurting while cycling?
To help improve your hip pain while cycling, it is perhaps most important to consider how you take care of your body when you are NOT cycling. The hip flexors and quads are used consistently and may become overworked and painful over time. Helping these muscles recover by adding in exercises to stretch and release tension in these muscles can help assist with recovery. Additionally, strengthening some of the opposing muscles (like the glutes and hamstrings) can help support a healthy muscle balance and keep the hips feeling strong and healthy.

Sciatica Pain Relief While Sitting: A Surprisingly Simple Natural Remedy
There’s no way around it – we’re living increasingly sedentary lives. That should come as no surprise in a world where you can order groceries, call friends, call a cab, and get in a full day’s work, all without leaving your chair.
Sitting down for long periods of time has become virtually unavoidable. And with sitting, unfortunately, can also come back and sciatica pain. As harmless as it seems, the simple act of sitting can cause excruciating pain, and nerve pain is no fun. Let’s find out why that happens and what you can do about sciatica pain from sitting.
Why does sitting cause back pain?
In theory, sitting sounds like it should be a great way to ease pain. You’re not up and around, and your body is at rest. That’s not the case, though – our bodies are made to be up and about, and excessive sitting can put a lot of pressure on your back, hips, and tailbone.
Dr. David Petron, a sports medicine physician, noted in an interview at the University of Utah that “the most common reason [for sciatica and lower back pain] is really prolonged sitting. We’re not designed to sit for hours at length.”
Lower back pain and sciatica from sitting is due to the amount of pressure being put on your disks. Sitting puts more pressure on the discs in your back than nearly any other activity, including running, especially if you are sitting with poor posture. These discs, when compressed, can hurt and can also press on the nerves coming out of the spine and cause pain. Sitting also creates increased pressure on the sciatic nerve in your glute, which travels all the way down to your leg. If you’ve ever felt shooting pains in your leg after sitting down, the issue may actually lie in the discs and nerves in your lower back.
Difference between lower back pain and sciatica
To make it clear: sciatica and lower back pain are not the same thing. More accurately, sciatica is one of many types of lower back pain, and it involves pain in the sciatic nerve that runs from your lower back down the outside of your thigh to the outer part of your shin. So, yes, you can have either lower back pain or sciatica from sitting – or both.
Although you may be feeling pain in your back or in this nerve that travels down your leg, the most common cause of this pain actually exists on the front of your hip. The hip flexor group, made up of your iliacus and psoas, works very hard to hold you in a sitting position whenever you are seated. Unfortunately, there is no best sitting position for low back pain or sciatica. The act of sitting is the cause of the problem. Getting up, moving around, and decreasing the time you sit is the only remedy for sciatica pain.
As a result of its extended workday and the shortened position in sitting, the hip flexor group is almost always tight, holding this tension even after you’re done sitting. This tension pulls on the spine, discs, and creates tension in the glute area. Like tug of war, the hip flexor tension on the front of the hip creates tension in muscles – like the piriformis – on the back of the hip, resulting in compression of the sciatic nerve as it travels through that muscle. This chronic compression is what causes sciatica and possibly low back pain.
There are so many reasons for this nerve and the spine to be unhappy when sitting. It’s a trainwreck. But it doesn’t have to be! Keep reading for some sciatica pain relief tips.
How do I get my sciatic nerve to stop hurting from sitting?
The solutions to get rid of your sitting-induced lower back pain are wide-ranging. In some cases, simply walking around and stretching can be a quick fix for the pain. This sounds simple, but many times, sitting is simply the reason for the pain. Prevention is the key. Getting up out of your chair every 30 minutes and stretching gives these parts of us the much-needed rest and increased circulation that is necessary to keep the body healthy. Set a timer or you will forget, trust me.
Fixing your sciatica and back pain problems isn’t always that simple, though. Many times, pain in the sciatic nerve can be aggravated by sitting, when the real cause lies elsewhere. Like I mention in my book, tight iliacus and psoas muscles (your hip flexors) can put the pelvis out of alignment, putting pressure on your sciatic nerve at the spine and the glute and causing pain.
How to relieve sciatica pain
Best stretches for sciatica
If you’re able to release some of the tension in your iliacus and psoas muscles, you give the sciatic nerve an opportunity to heal. The Hip Hook is designed specifically for this purpose. This prolonged pressure technique is the golden ticket to long term change in the holding patterns of this muscle, however, stretching can be a great way to prevent and soften these effects in the moment.
Since piriformis tightness develops as a result of fighting against the tension in the iliacus and psoas, stretching this area can relieve the tension of those muscles and therefore reduce pressure on the sciatic nerve. First, you want to address the hip flexors with a hip flexor stretch as that is the hidden cause of sciatic tightness. Then address the effect by stretching the piriformis with a figure 4 stretch. Holding each stretch for at least 30 seconds will help soften the hold that these muscles have on you!
Self massage for sciatica
While the piriformis lies underneath the larger gluteus maximus, it is still relatively close to the surface of the body. This helps make the muscle easier to access by using something like a foam roller, lacrosse ball, or a massage therapy ball. Self massage for sciatica is more about applying prolonged pressure to release these muscles than kneading them with your hands.
While self massage for sciatica pain relief may hurt, it should be more of a “hurts so good” kind of feeling during and after the release. The pain should start decreasing after 30 seconds; if it doesn’t, move the tool to a different spot. If at any point you feel a large increase in pain that lingers after the release, you may want to reduce the intensity of the pressure and/or explore a different spot along the muscle. If that increased pain does not go away, please stop and consult your healthcare practitioner.

Do I need surgery for my lower back pain and sciatica?
One common issue that’s prevalent throughout our culture is that surgery is necessary – and beneficial – in cases where there’s significant pain. While this is true in some cases and you should always consult with your doctor, sciatica and lower back pain typically does not require surgery. The key to determining if you need surgery is to first determine the actual cause of your pain. Just because you have a herniated disc, doesn’t mean that it is the source of your pain. There are many people, young and old, that have herniated discs with no pain.
Sitting and sciatica pain relief
Instead, physical therapy is normally the best way to treat the lower back pain and sciatic problems that you’re having. Whether you simply need to get in a yoga routine, specific stretches, or to release tension in your hip flexors, physical therapy can offer a lot of solutions that surgery cannot – with the added benefit of being much less risky and more beneficial overall. Try PT first!
Back pain and sciatica issues from sitting are quite common, and they’re continually becoming more commonplace as so many jobs and lifestyles involve sitting for long periods of time. If you’re able to, try to get up and be active as much as you can, and simply taking a walk around the block can make all the difference! This will help to prevent these issues from occurring in the first place.
Best sitting positions for sciatica
In addition to getting up more frequently to move around, try mixing in some different positions to figure out what the best sitting position is for YOUR body to relieve your sciatica pain. We’ll share some ideas on how to sit with sciatica below, which you may use to get some short-term relief as you keep working towards addressing the root cause of your pain for long-term results.
1. Sitting with a more open hip angle
A common sitting position for many people is where the height of the seat allows for their feet to be flat on the ground and also have the knees and hips at about a 90-degree angle. This places the hip flexors into a shortened position (compared to a 180-degree angle when standing) and increases the chances for tightness that ultimately contributes to sciatica.
Assuming that a standing desk isn’t available or you aren’t able to stand for 8+ hours straight during the day, the next best option would be to sit with a more open hip angle. This could be achieved by raising the height of your chair, placing a cushion on top of your chair, tucking your feet underneath your chair, or even utilizing a kneeling chair (if you have one).

Each of these positions opens the hip angle to more than 90 degrees and helps to lengthen the hip flexors, giving them a chance to relax a little more and hopefully take some pressure off of the sciatic nerve being irritated. If you have a soft mat that you can lay on the floor and if the height of your desk allows for it, you could take this one step further and take a kneeling position or half-kneeling position (like a kneeling hip flexor stretch) while you sit to open up both (or just one) of your hips to a 180-degree angle.
2. Sitting cross-legged or with one leg crossed over the other knee
Whether you find yourself seated in a chair, car, couch, or even on the ground, a possible way to sit with sciatica and get some relief would be to sit cross-legged or have one leg crossed over the other knee (very similar to the Figure 4 stretch). Doing so will stretch the piriformis muscle which, when tight, can irritate the sciatic nerve that runs directly underneath it. Sitting this way may help lengthen that muscle, reduce the compression on the nerve, and provide you with some relief.
3. Sitting with some lower back support
Giving the lower back some support, whether it is by using a lumbar roll cushion or sitting in a chair with built-in lumbar support, can help provide your muscles with enough help to let them relax a little more to take enough pressure off of the sciatic nerve so that you can experience some relief.
Frequently asked questions on sciatica while sitting
Does sitting make sciatica worse?
Sitting too much, especially for longer periods of time, can be something that triggers or worsens your sciatic pain. When sitting, the muscles that support the alignment of your pelvis and lower back can become tighter and compress on the sciatic nerve. Taking frequent breaks to move around or stretch may help to relieve the tightness in this area and reduce the pain.
Where does the sciatic nerve run?
The sciatic nerve starts in the lower back and runs through the hips and buttocks (underneath the piriformis muscle) all the way down the legs.
What causes sciatica?
Sciatica is caused by a compression on the sciatic nerve, which branches through the lumbar spine and runs through the glutes and all the way down the legs. Compression on the nerve can happen in several ways, such as a bulging or herniated disc, pinching of the nerve by decreased space in the lumbar spine, or from tight muscles (like the piriformis) pressing on the nerve.
How do I get my sciatic nerve to stop hurting?
To improve your sciatica pain, it is important to first find the true root cause of your pain. Sciatica may develop over time as the result of muscle imbalances around the pelvis and lumbar spine. This impacts the alignment of the structures and function of the muscles in these areas, ultimately compressing on the sciatic nerve and causing pain. Using a combination of muscle release and corrective stretching and strengthening exercises, you may be able to improve the alignment of your body and the functioning of the supporting muscles, addressing that root cause to improve your sciatic pain.

Yoga for Tight Hip Flexors: Stretch Safely, Stay Healthy
Yoga is a great way to stay in shape, but like any exercise, it comes with its own set of dangers. If you’ve got hip pain, it’s important to make sure the yoga you’re doing is compatible with your hip flexors.
Don’t worry: you probably won’t have to overhaul your yoga routine, but you might be able to solve a lot of your hip pain by identifying the root cause and figuring out solutions to solve it.
Read on to learn a little bit more about why yoga might be causing your hip pain, and what you can do about it.
The dangers of hip opening yoga
First, let’s establish what your hip flexors actually are. The hip flexors are a group of muscles on the front of your hips that help move your leg forward; the two major hip flexor muscles that are often the culprits of pain are the iliacus and the psoas (known as the iliopsoas), and that’s what I’ll be focusing on here.
In yoga, hip flexor stretches are commonly overdone. Yoga “hip openers” are the norm and everyone feels like their hips are so tight because they experience the sensation of stretching when they stretch their hips in poses like pigeon, forward folds, and butterfly. The problem is that the hip joint is designed to be mobile and stable and having somewhat less flexibility around the hip can actually stabilize the joint. Continuing to build flexibility in this area can be too much of a good thing.
What causes tight hip flexors?
You may feel like your hip flexors are good because you can go deep into a lunge pose and barely feel a thing. Muscles can hold tension and still allow for stretching. Once the joint becomes unstable with more and more stretching, paradoxically the iliacus and psoas begin to hold tension and develop knots in an effort to stabilize the hip joint. These knots do not necessarily limit your range of motion. You can notice this when your hip flexor muscle is holding tension even at rest. This is one indication that this muscle is trying to hold you together.
This tension not only causes pain and discomfort around the hip, tailbone, and spine, but it can affect the entire leg and even work its way up the spine to the shoulder and neck. In addition, overstretching of the hip can end up putting strain on the joint capsule and muscles that hold the joint together, leading to sore hips after yoga. Continuing this pattern of forcing yourself into deeper poses puts awkward and unnatural stresses on the joint, resulting in more instability and wear over time. This is how you end up with more hip pain and an increased chance for injury during or after yoga, which is the opposite of what you are looking for.
Additionally, many yoga poses require an abundance of strength and endurance of the iliacus and psoas. When a muscle is holding excess tension all day long in an effort to stabilize the joint, it is not happy when it is additionally asked to work. It’s already exhausted. Take these yoga poses, for example: staff pose, boat pose, extended hand to big toe pose.
All of these poses have one thing in common: they put excessive stress on the iliopsoas because they rely on it for strength. This can aggravate the muscle, lead to sore hips after yoga, and cause pain. If there is underlying tension, then these poses will contribute to increasing the pull of these muscles and contribute to pelvic rotations and misalignment of the entire body.
There is one more major piece to the puzzle. Any activity where you have one leg going forward and the other going back increases the chance your iliopsoas will tighten up; this is because this type of stance can pull your pelvis out of alignment, especially if you are starting with tension in the iliacus or psoas to begin with. The problem typically gets worse as you push deeper into the pose – but that doesn’t mean you have to stop your yoga exercises entirely. Keep reading to learn how to avoid hip injuries while doing yoga for tight hip flexors.
What are the symptoms of a tight iliacus or tight psoas?
If you’ve got problems with your hip flexors, you might experience a few other issues when doing yoga. A tight iliopsoas affects the alignment of your hip and SI (sacroiliac) joint, causing the hip to awkwardly shift in the socket, which can sometimes make a strange clunking noise. You might notice this noise during yoga, particularly during poses like the triangle pose, leg lowering poses, or the extended hand to big toe pose.
Hamstring tendonitis is another unintended and quite painful side effect of tight hip flexors. If you’re during yoga poses that stretch your hamstring while the hip flexor is also pulling you forward due to its tightness, you might create a tug of war scenario, putting undue stress on the hamstring and causing tendonitis.
How can I prevent tight hip flexors with yoga?
Even though yoga can increase the chances of a tight iliopsoas and sore hips, that doesn’t mean you have to stop doing yoga entirely. There are plenty of ways to practice yoga in a safe and healthy way that prioritizes strengthening your hip flexors rather than overstretching them.
One of the best ways to prevent hip injury during yoga is to shorten your stance, and avoid pushing deep into the pose. The Warrior II pose is a perfect example: instead of going deep into the pose, try grounding by pushing down into the ground and pulling your legs towards each other to engage the deep hip stabilizing muscles.

Another thing you can do as a preventative measure is to focus on strengthening your core and your hips – this will allow you to do more yoga poses as you get stronger. In my book about this tight hip phenomenon, I recommend Barre classes and core stability exercises to help stabilize your hips.
The bottom line? Yoga for tight hip flexors can be done in a way that’s safe and healthy for your hips, but you may have to modify some poses to make sure you’re giving your iliopsoas some rest.
Instead of implementing a drastic change to your routine, make simple changes along the way. Focus on posture and breathing instead of going into a deeper pose. Do the pigeon pose on your back instead of the full pigeon pose. Avoid exercises that involve one leg going forward while the other is going back. These are just a few of the many ways you can improve your hip flexor stretches and set yourself on a path for pain-free hips.
If hip pain isn’t the only problem you’re having, check out my article on the most common yoga injuries – and how to prevent them. And, if you’re interested in learning more about how you can solve your hip issues, that’s what my book, Tight Hip, Twisted Core is all about!
Frequently asked questions about yoga and tight hip flexors
Is yoga good for tight hip flexors?
Yoga can be helpful in loosening up your tight hip flexors, as well as the other supporting muscles around your hips. For the best and longest-lasting results, it is very important to work within a range of motion for each yoga pose that works for your body and also one which you can actively control.
Why do my hips hurt after yoga?
If you are experiencing more pain or tightness after doing some yoga poses, it may be because you are working into too large of a range of motion in your poses. While it may feel like you are getting a nice stretch by going as deep into a yoga pose as possible, your hip flexors and other hip muscles could actually be holding tension to create stability around your hips, pelvis, and lower back.
How can I prevent injuries during yoga?
To prevent injuries during yoga, it is important to work within a range of motion that you can actively control. For many yogis (especially beginners), that means shortening your stance during yoga poses and making sure that your muscles are engaged to support you in that position. If you try to go too far into a yoga pose, this can cause over-stretching your muscles, tendons, ligaments, and joints past what they are currently capable of, thereby increasing the risk of pain, tightness, or injury.
Why do I have sore hips after yoga?
If you are experiencing a lot of hip soreness after yoga, it may be because you are forcing your body into too large of a range of motion than your muscles are currently able to hold. While it may seem like you are performing a pose well and feeling a big stretch because you are going deeper into a yoga pose, you may actually be over-stretching your hips. This may cause the hip flexors and other hip muscles to hold tension in an effort to create stability and protect your body. The result is typically a deep soreness in the hips after yoga, which can increase your chances for injury over time as this pattern continues.